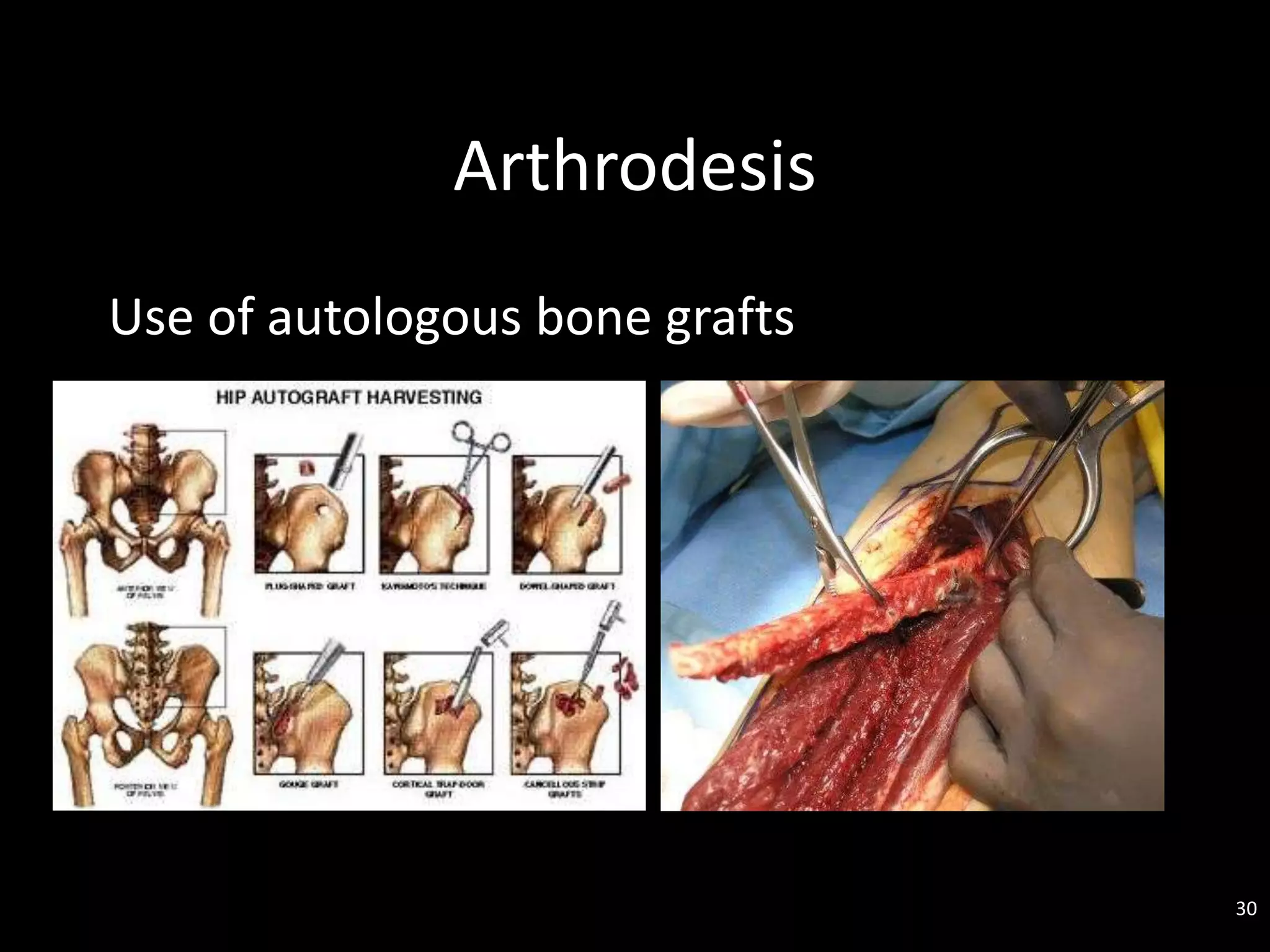
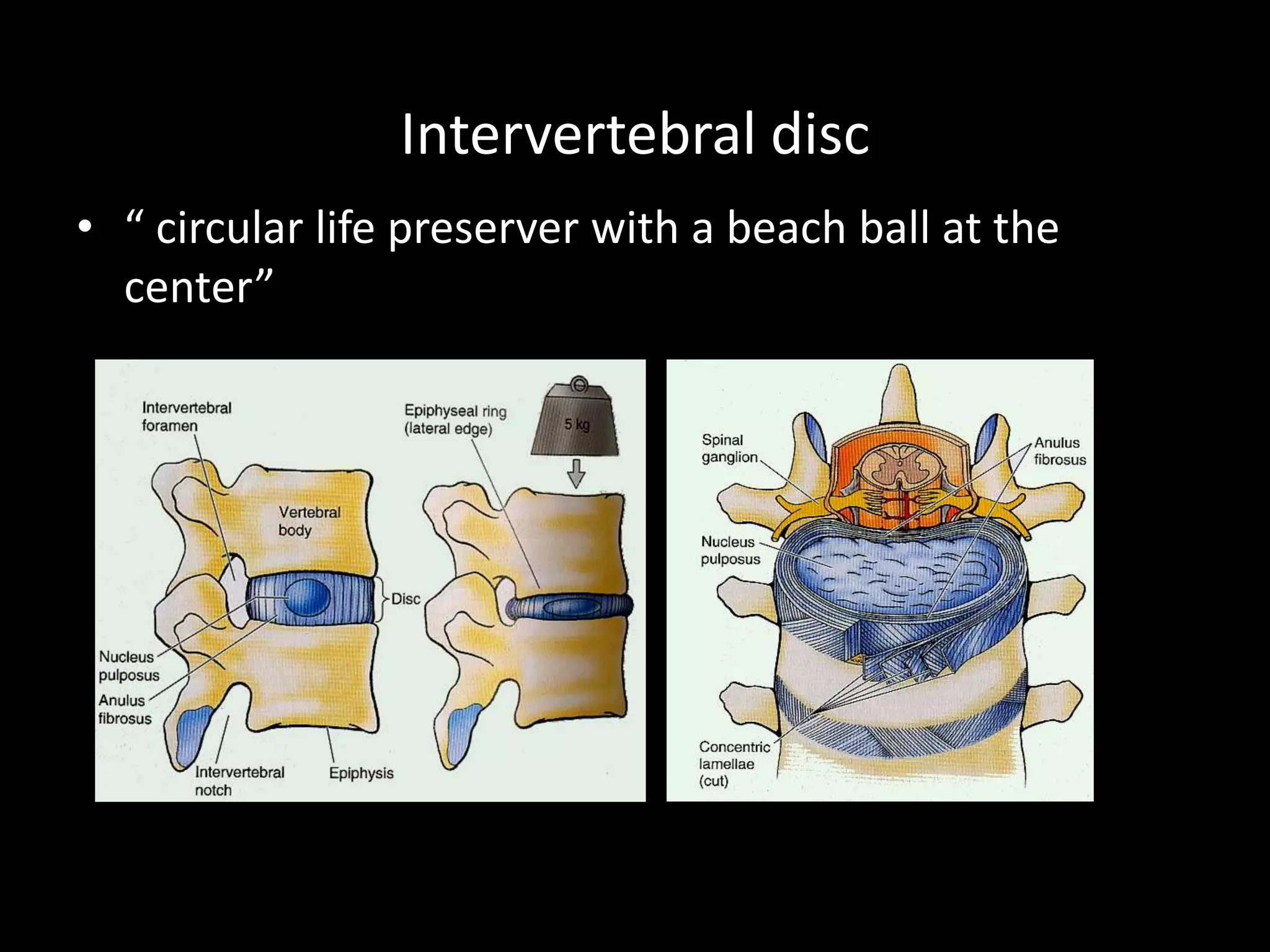
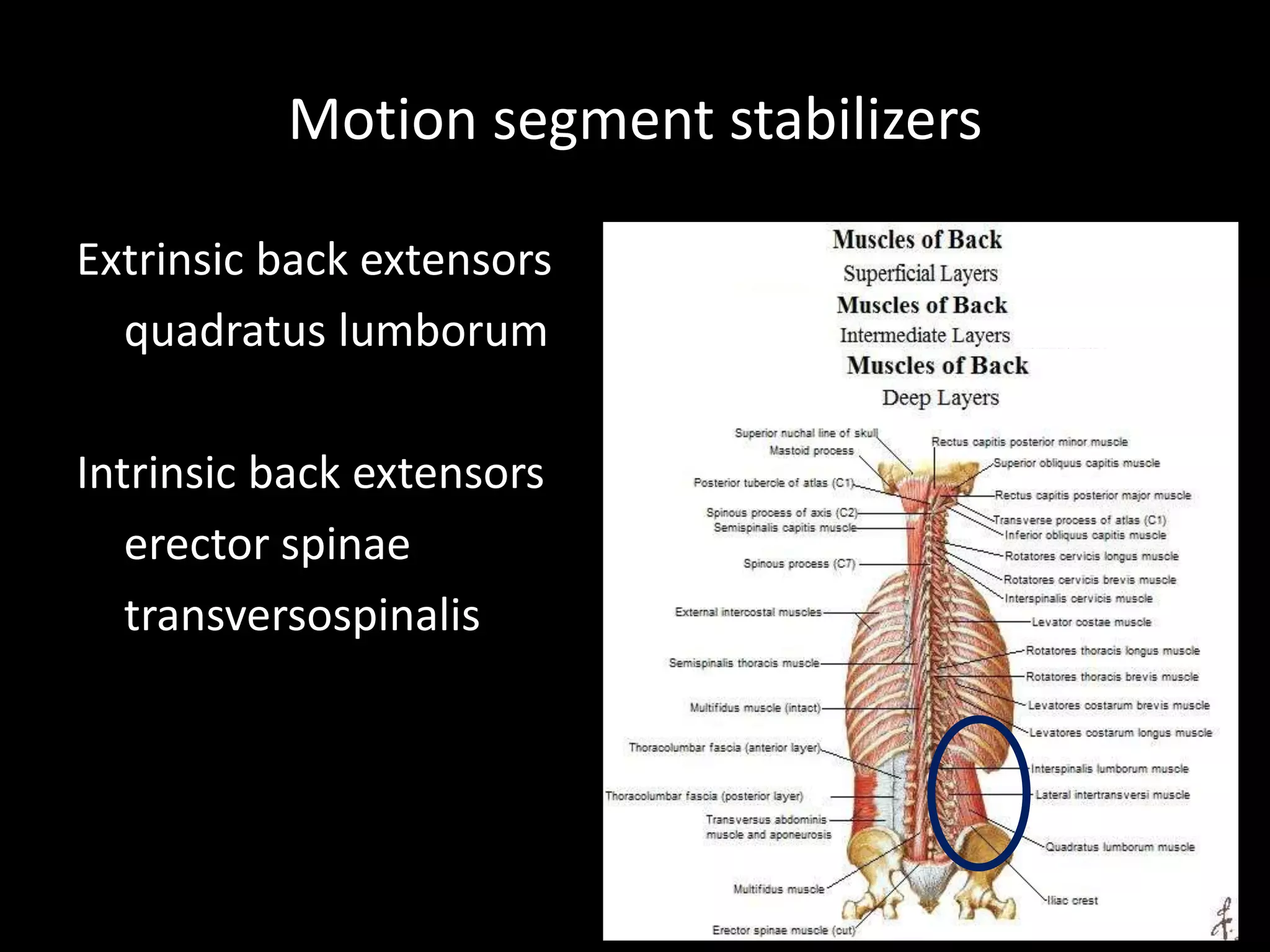
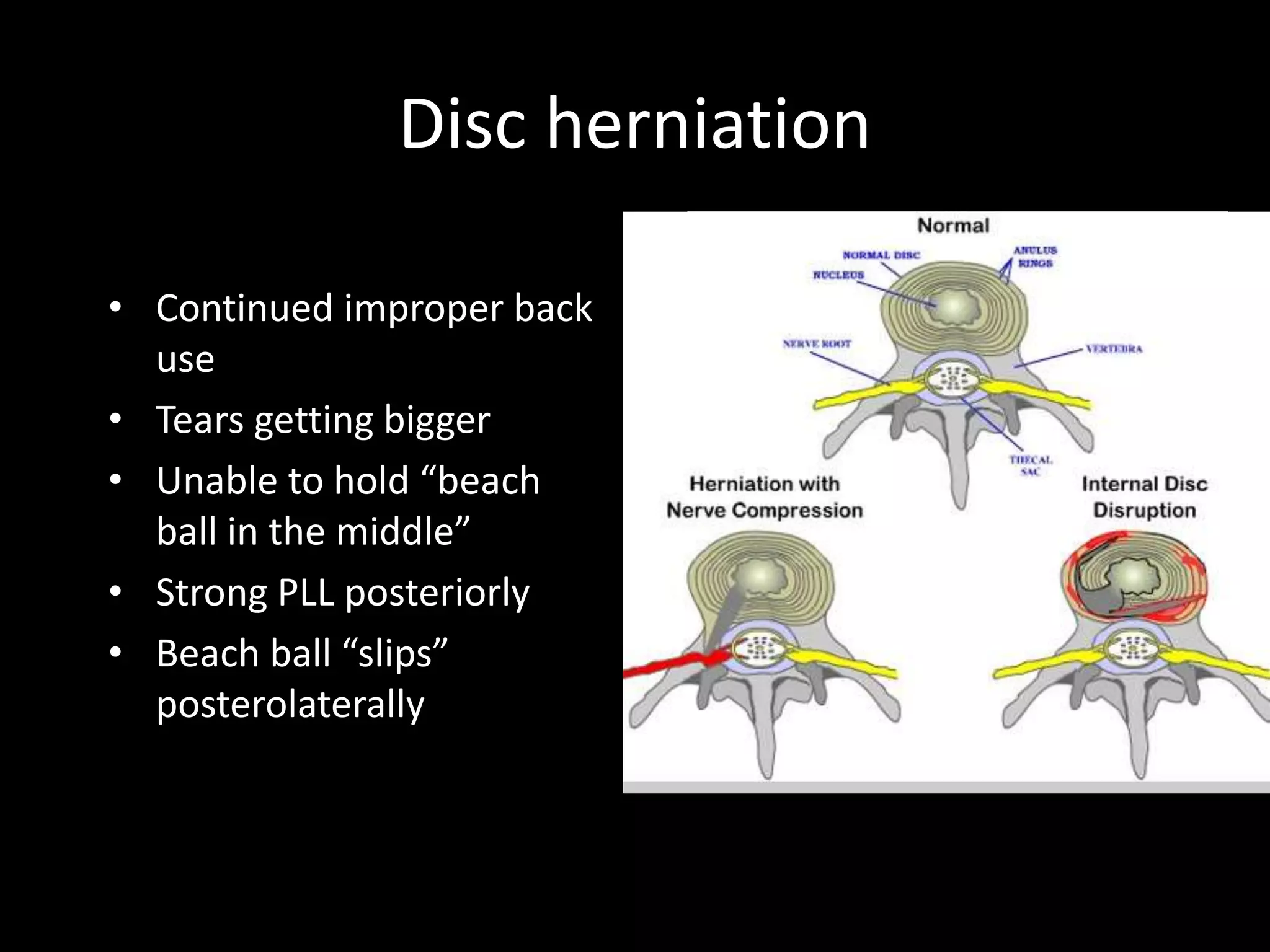
This document discusses disorders of the back, including clinical manifestations, causes, evaluation, and management. It covers common issues like back pain, disc herniation, spinal stenosis, and fractures. Evaluation involves history, exam, imaging like x-rays and MRI, and sometimes lab tests or biopsies. Management depends on the underlying problem but generally involves conservative options like medications, physical therapy, bracing, or surgery for decompression or fusion in cases of neurological compromise or failure of conservative care.