This document provides an overview of carcinoma of the cervix, including its anatomy, histology, risk factors, evaluation, staging, and treatment. Some key points:
- HPV infection is the main risk factor, with some high-risk HPV subtypes associated with 95% of cervical cancers. Vaccination can prevent HPV infection.
- Evaluation involves Pap smear, colposcopy if abnormal Pap, and biopsy for diagnosis. Staging includes physical exam, imaging like CT/MRI, and FIGO clinical staging.
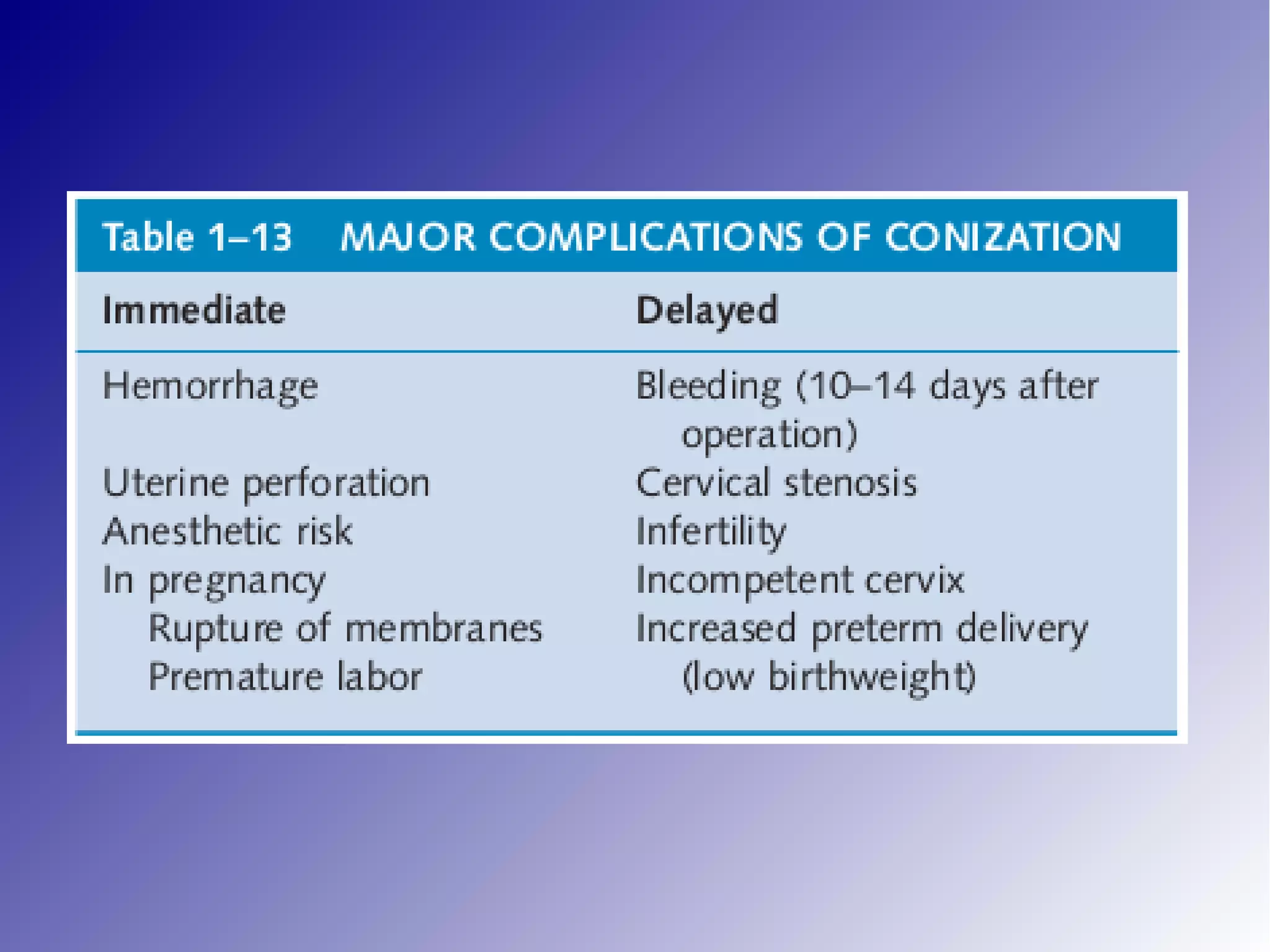
- Early lesions are treated with LEEP or conization. Advanced invasive cancers are staged surgically with radical hysterectomy and may involve chemotherapy or radiation if disease has spread. Regular screening can