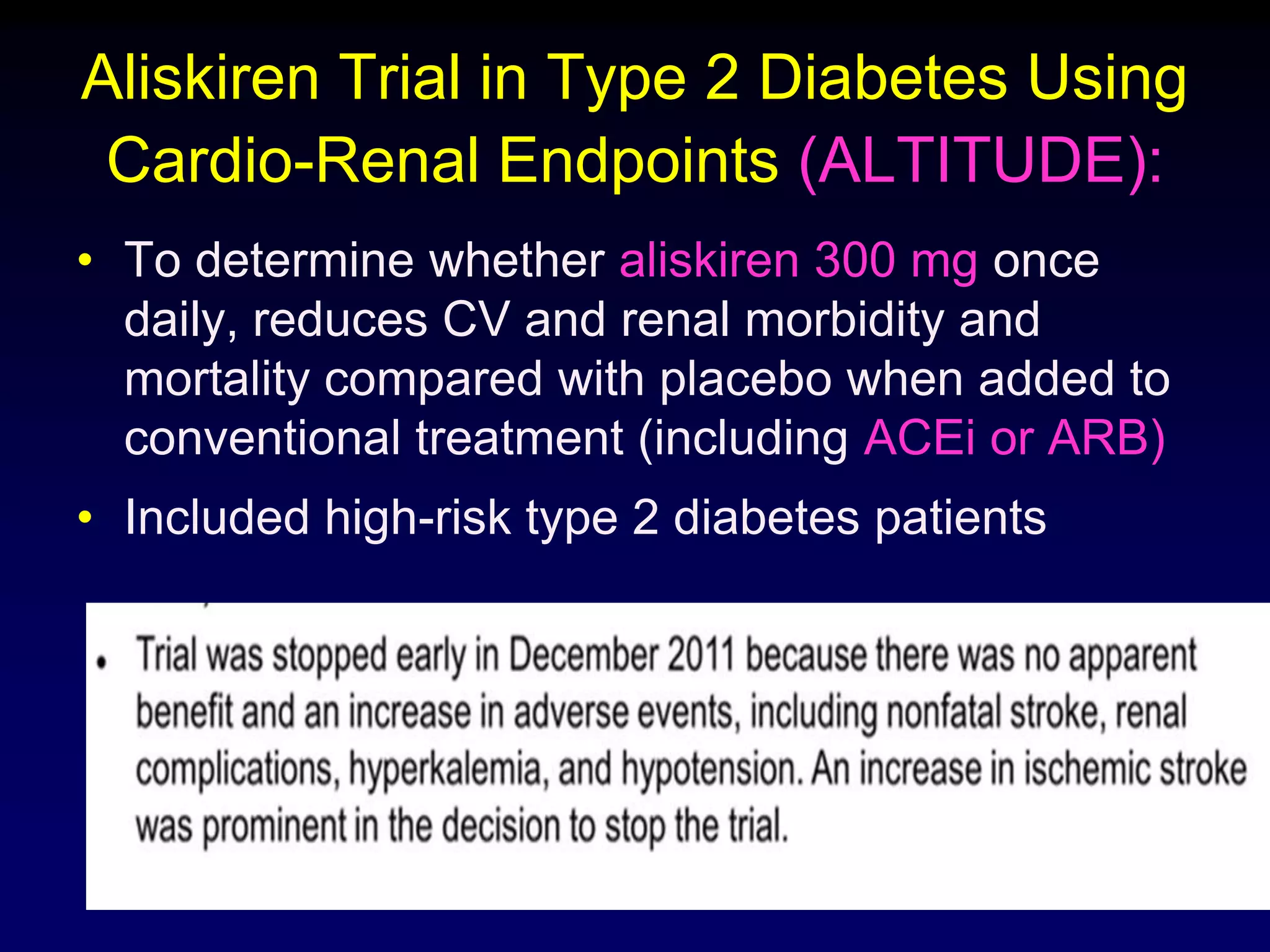
Diabetic nephropathy is a leading cause of end-stage renal disease worldwide. Strict control of blood glucose, blood pressure, angiotensin system inhibitors, and other risk factors can help prevent or slow the progression of kidney damage. The stages include early hyperfiltration, development of microalbuminuria, progression to macroalbuminuria and renal failure. Management focuses on glycemic control, blood pressure reduction, angiotensin blockade, cholesterol control, and management of anemia and cardiovascular risk factors to preserve kidney function for as long as possible.
































































































![Diabetes
Asymptomatic bacteriuria is more common
(20%)
UTIs are likely to be more severe in diabetic
than nondiabetic women
Asymptomatic bacteriuria often precedes
symptomatic UTI in type 2 diabetes [RR]
1.65
Risk factors for UTI in diabetics includes
those
who take insulin (relative risk 3.7)
longer diabetes duration (>10 years, relative risk
2.6)
○ but not glucose control
Emphysematous pyelonephritis,
xanthogranulomatous UTI and fungal UTI are](https://image.slidesharecdn.com/diabeticnephropathy-management-130816073518-phpapp02/75/Diabetic-nephropathy-management-98-2048.jpg)