This document provides guidance on the long-term management of asthma in children and adults. It discusses:
- Inhaled corticosteroids as the mainstay of daily treatment, with short-acting beta agonists for relief of symptoms. Dosages depend on age and severity.
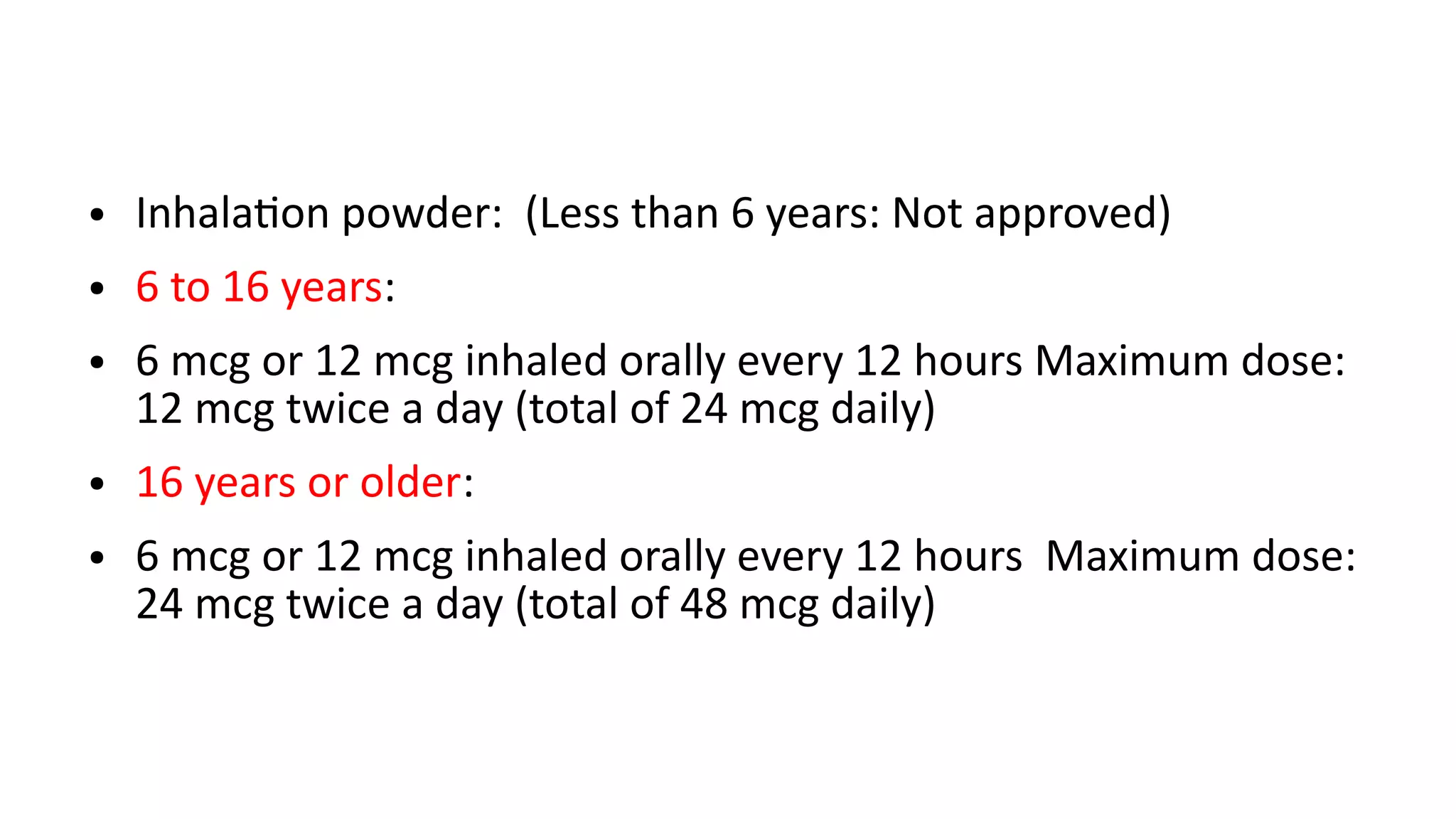
- For some children over 6, the addition of long-acting beta agonists. Children over 12 need adult dosages.
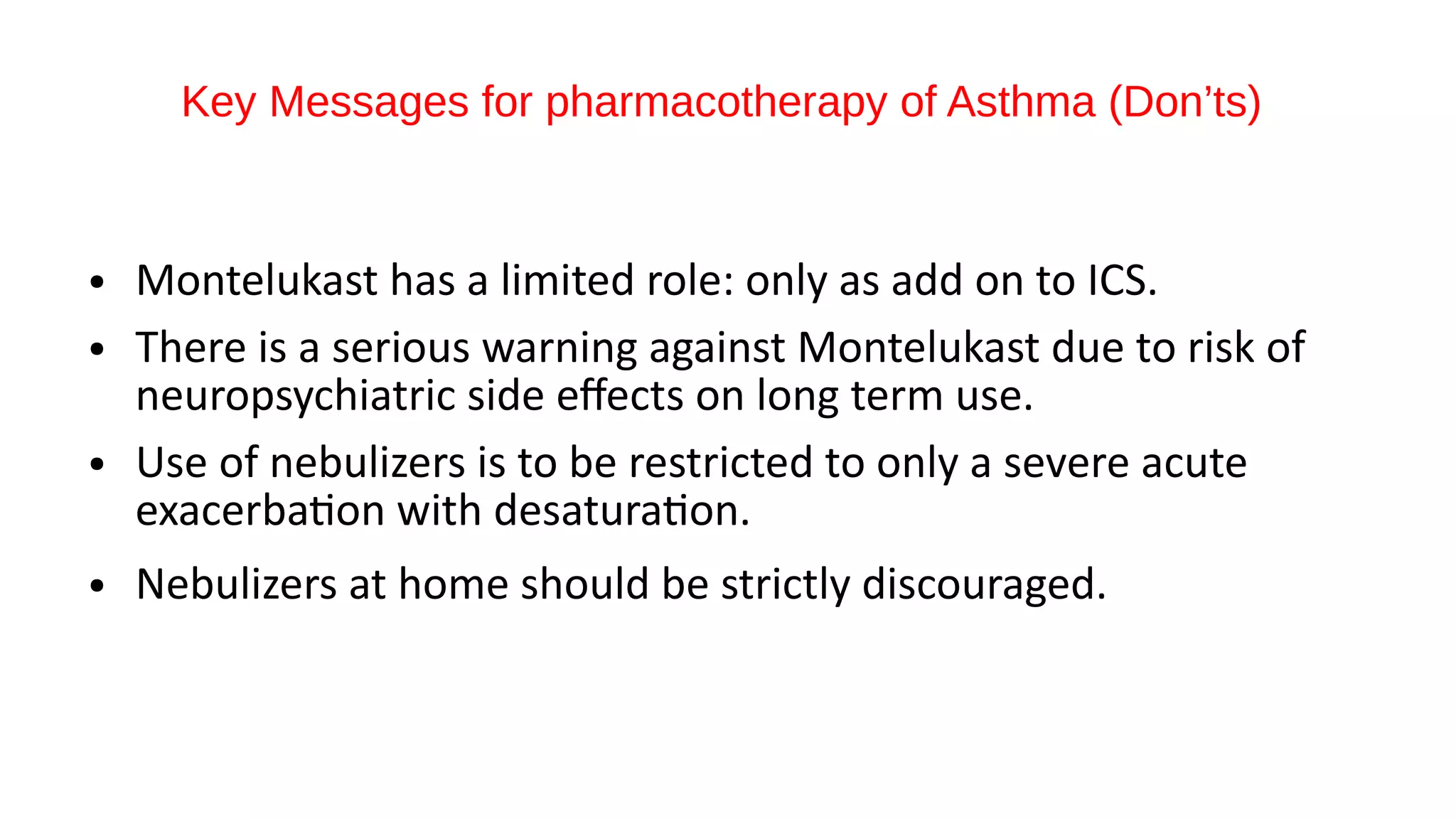
- Metered dose inhalers with spacers are preferred for all children. Montelukast has a limited role and there are warnings about its long-term use.
- Treatment is stepped up or down based on symptom control and future risk of exacerbations. Regular assessment and adjustment of the treatment