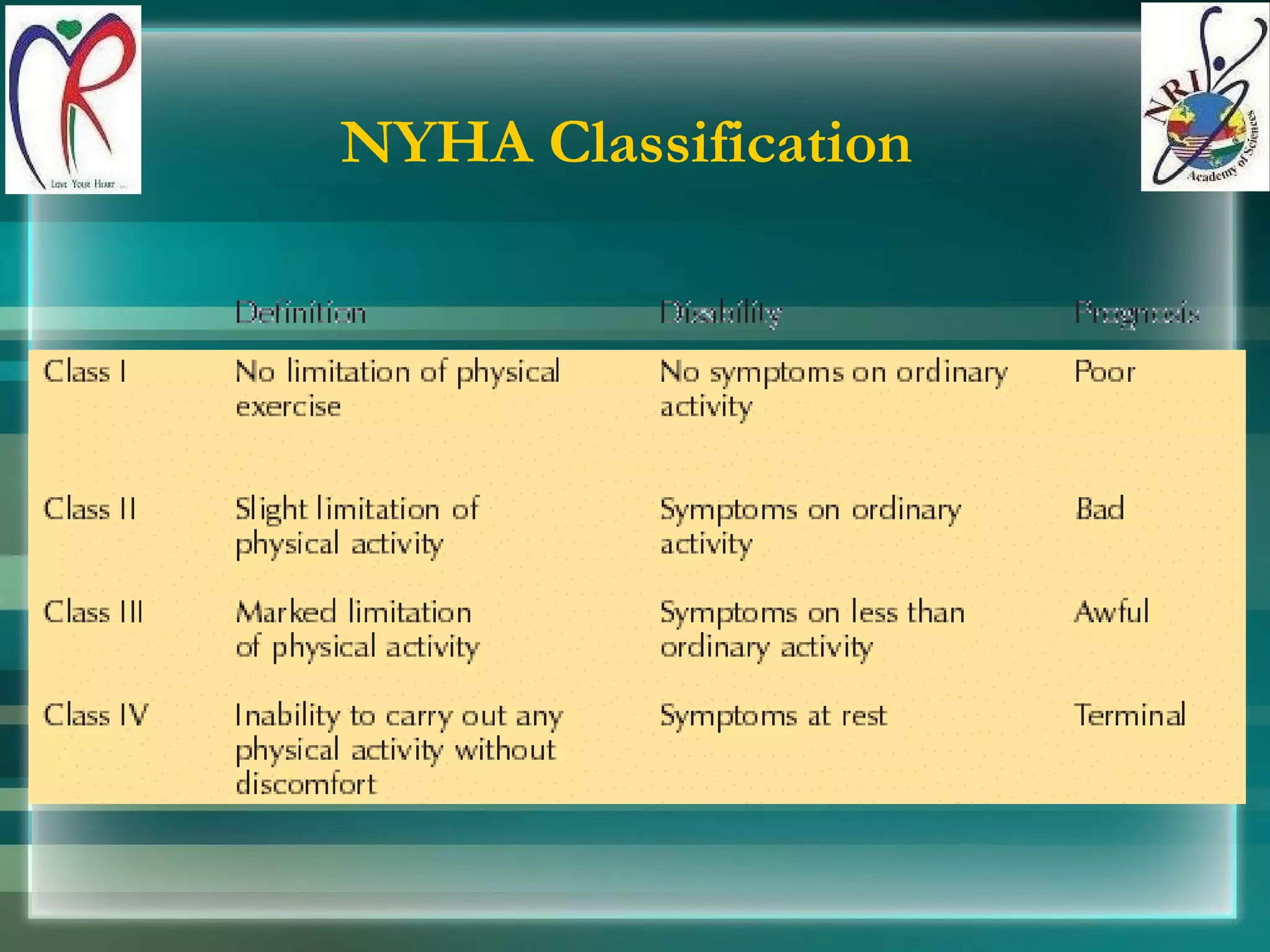
Heart failure (HF) is a clinical syndrome resulting from cardiac disorders affecting the ventricles' ability to fill or eject blood, with a higher incidence in older adults. It is classified into various types and stages to emphasize its preventability and progressive nature, with evaluations including symptoms and diagnostic tests. The Framingham criteria outline major and minor signs for diagnosing congestive heart failure.