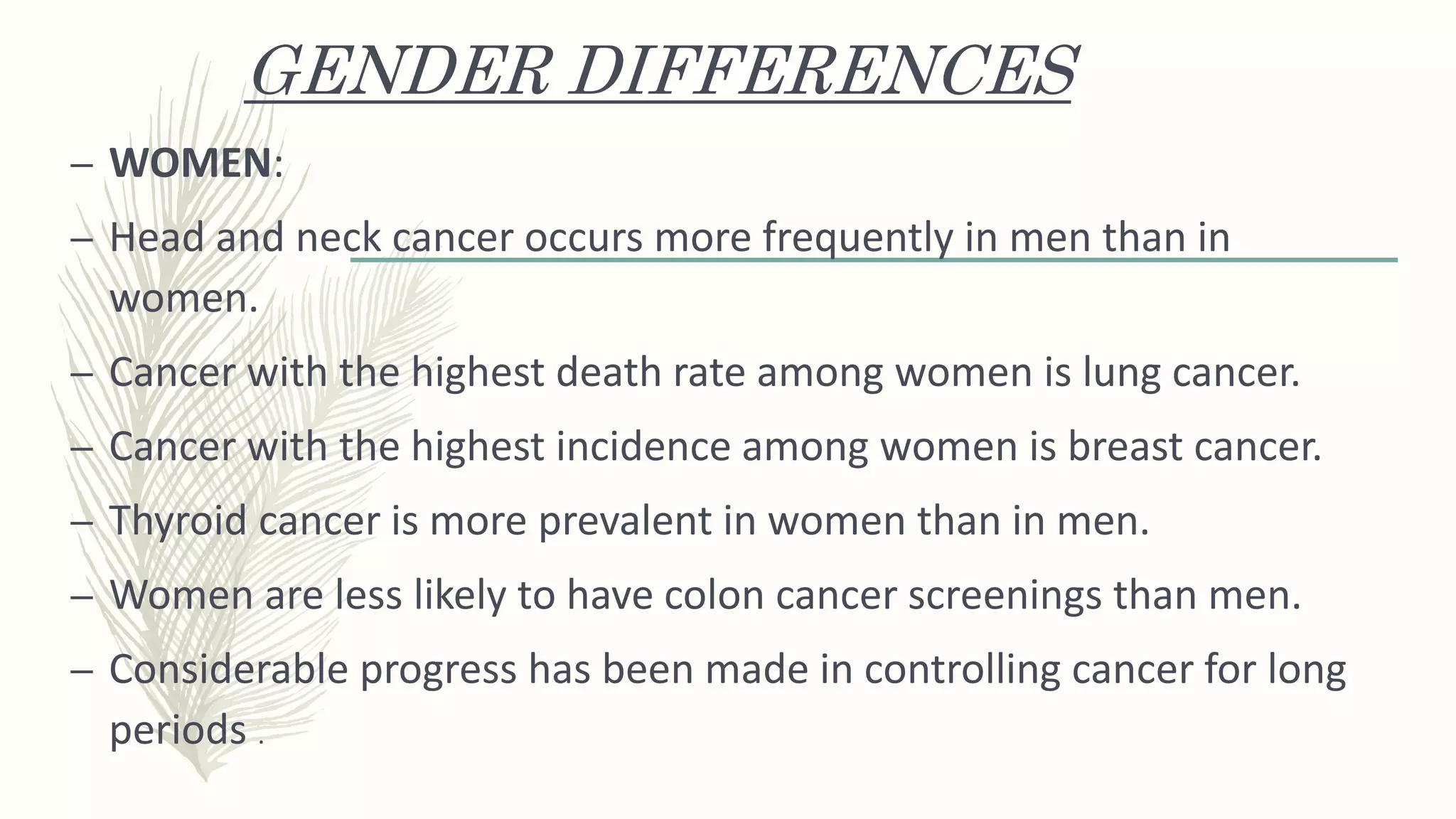
This document provides an introduction to cancer including definitions, types, causes, risk factors, screening recommendations, and diagnostic tools. It defines cancer as uncontrolled cell growth and outlines the differences between normal and cancerous cells. Common cancer types are described as well as factors that can increase cancer risk such as viruses, chemicals, radiation, genetics, and lifestyle choices. The document also discusses how cancers are classified and diagnosed.