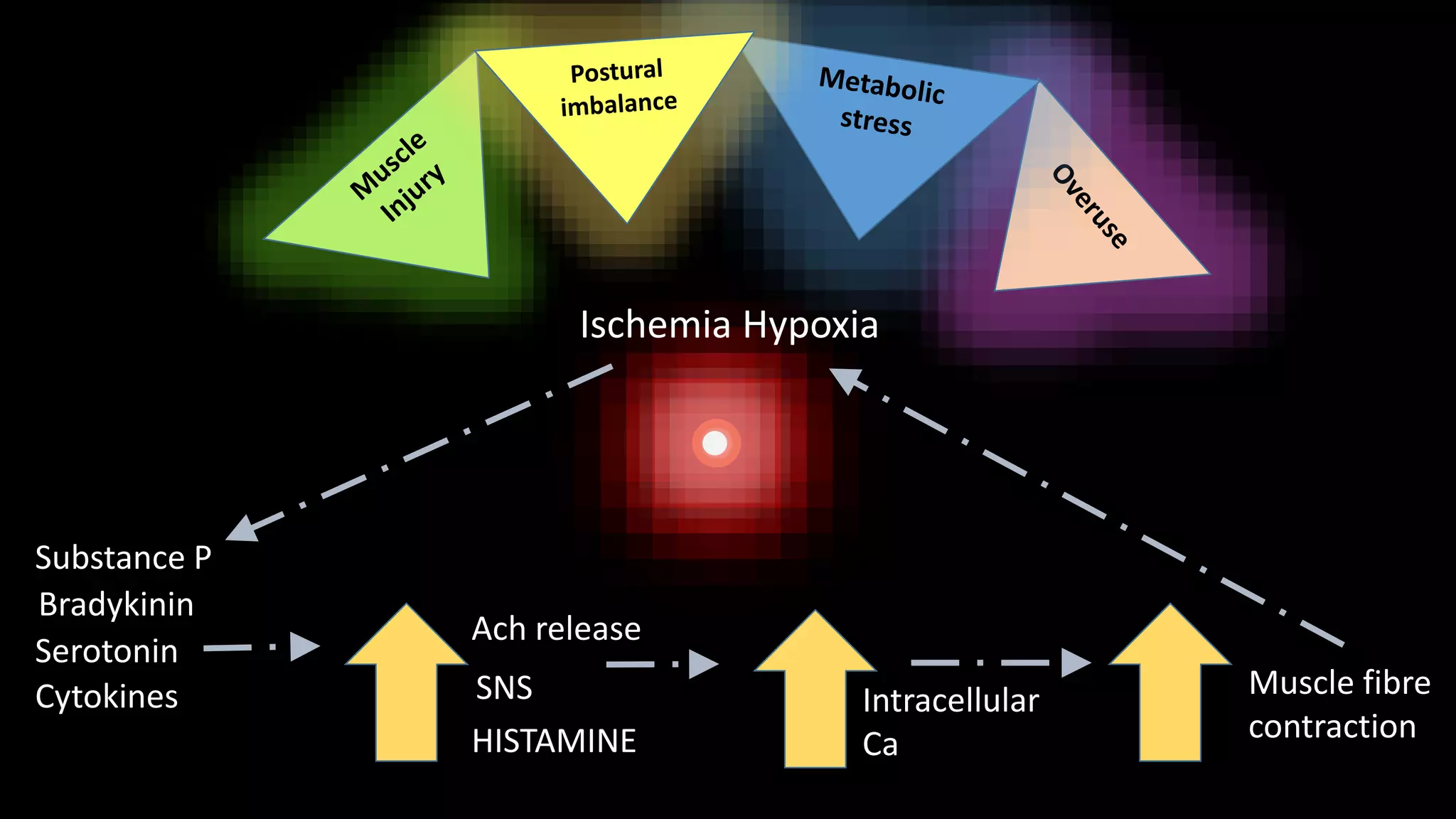
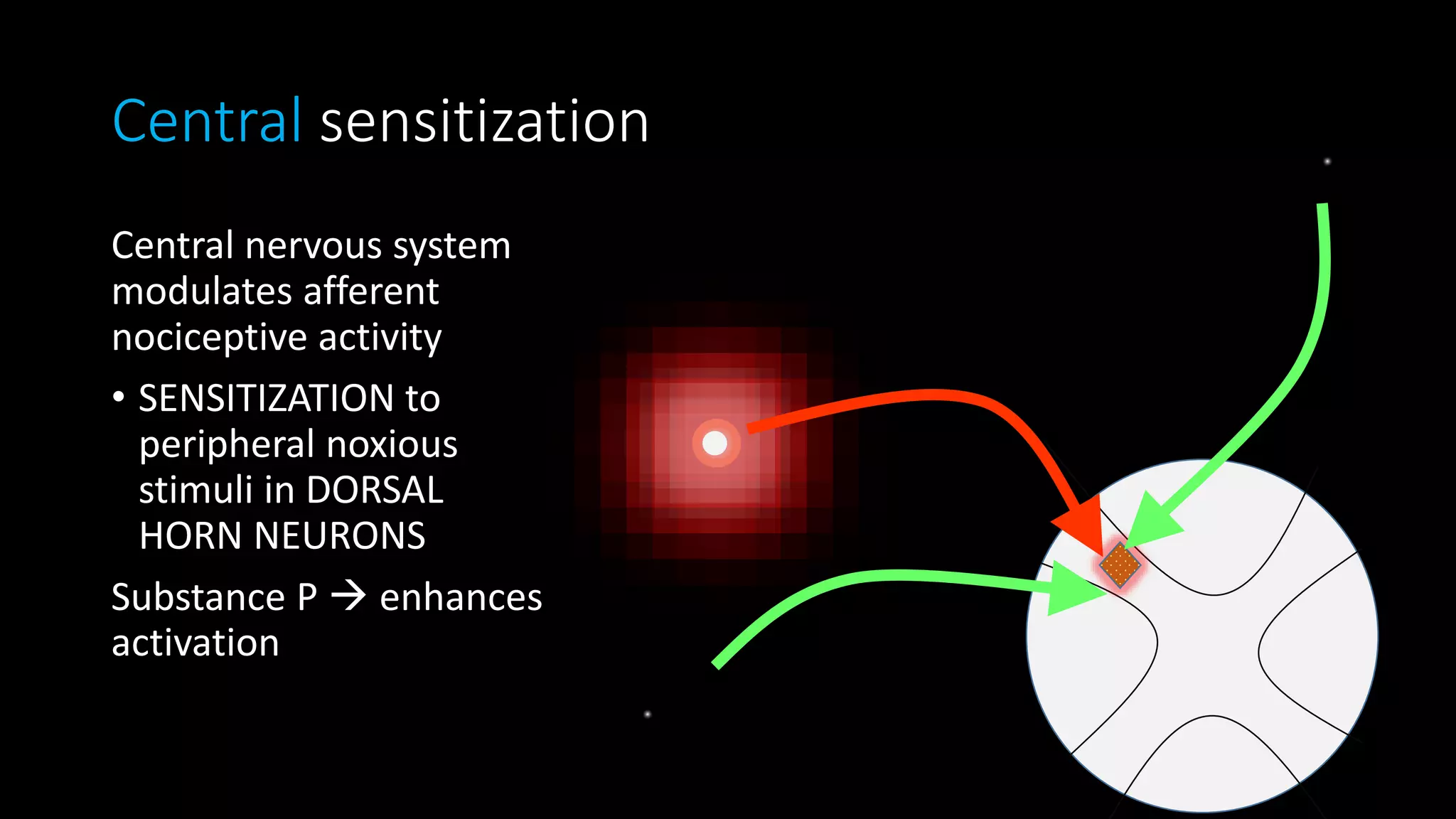
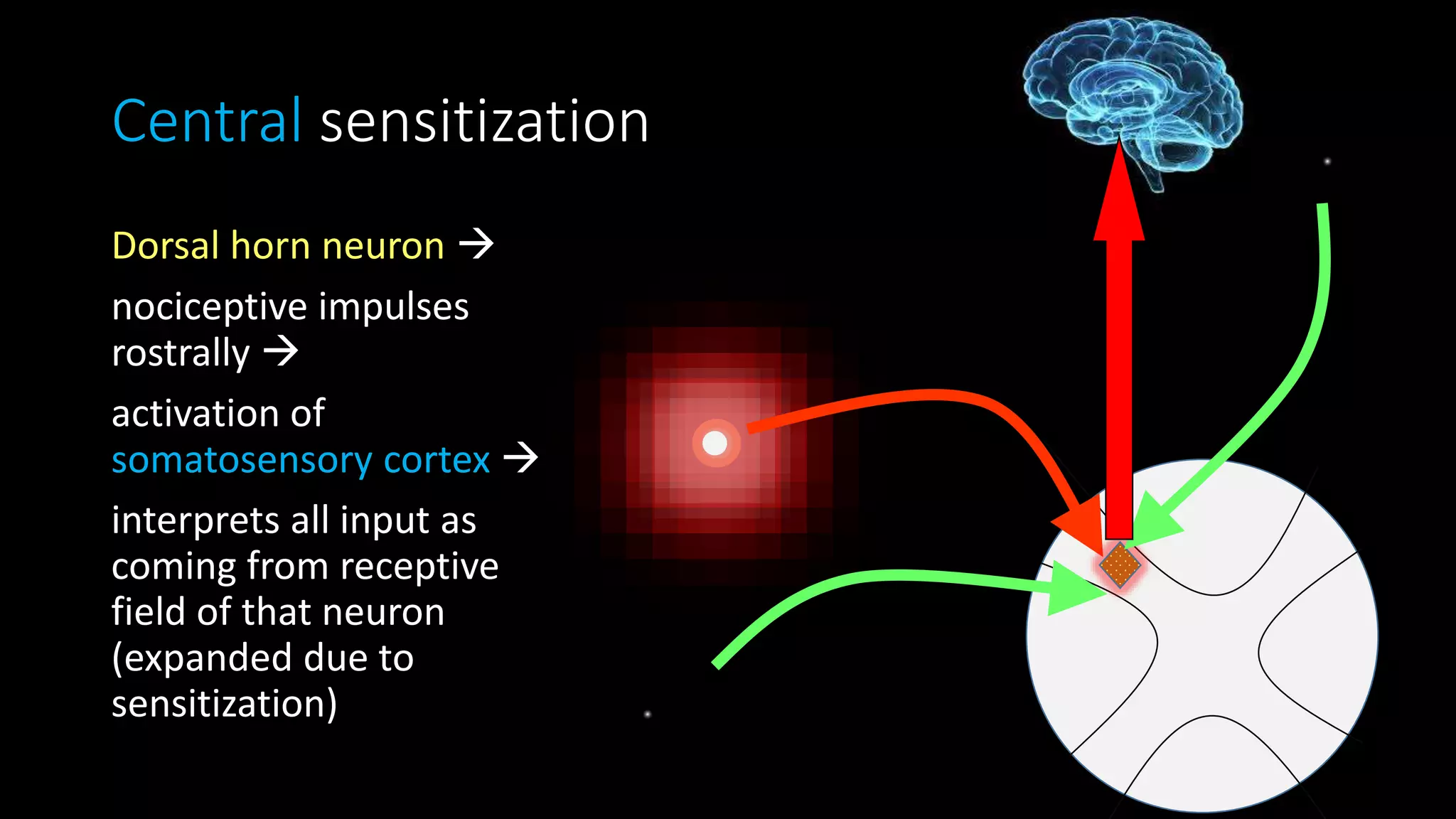
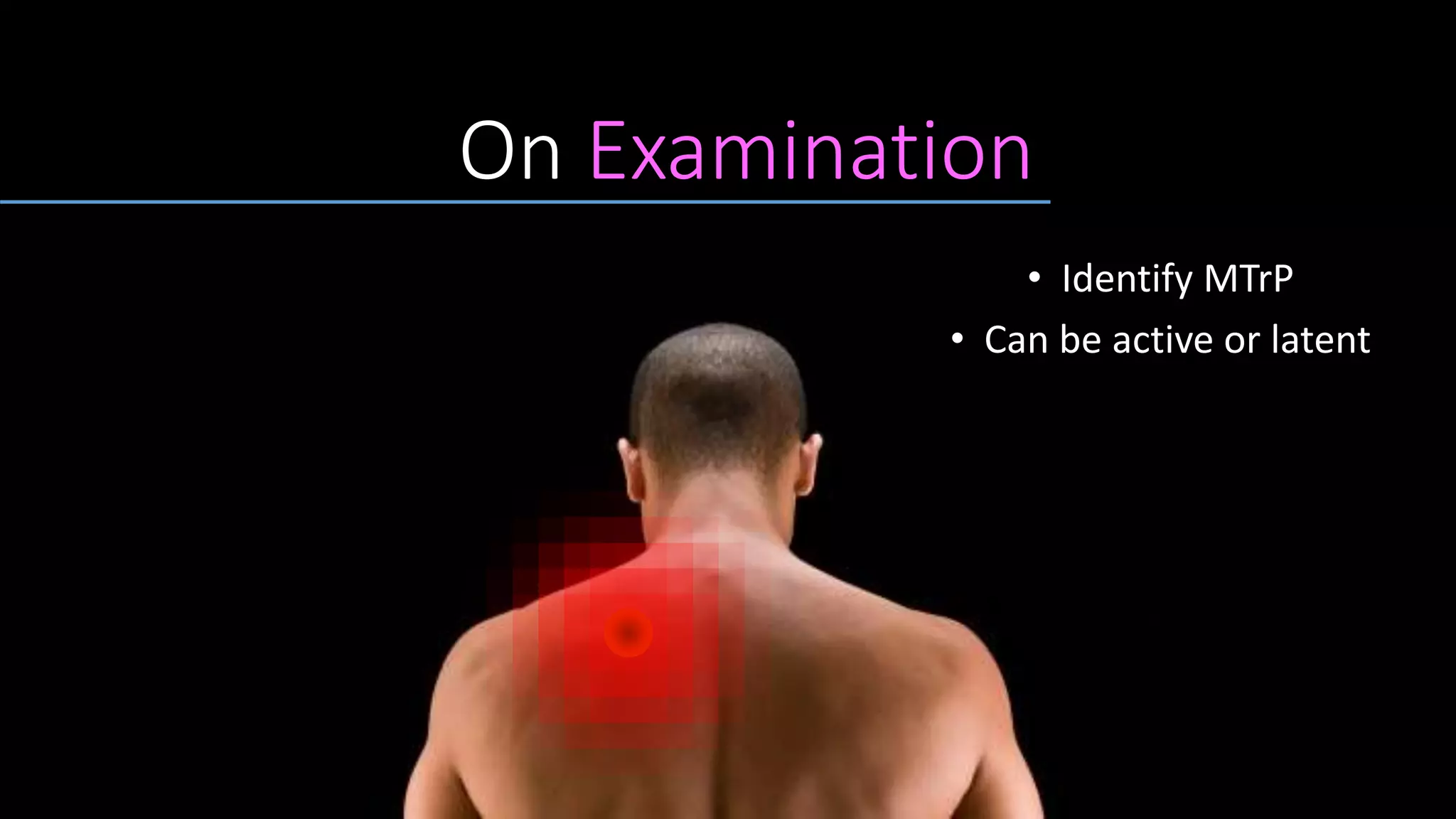
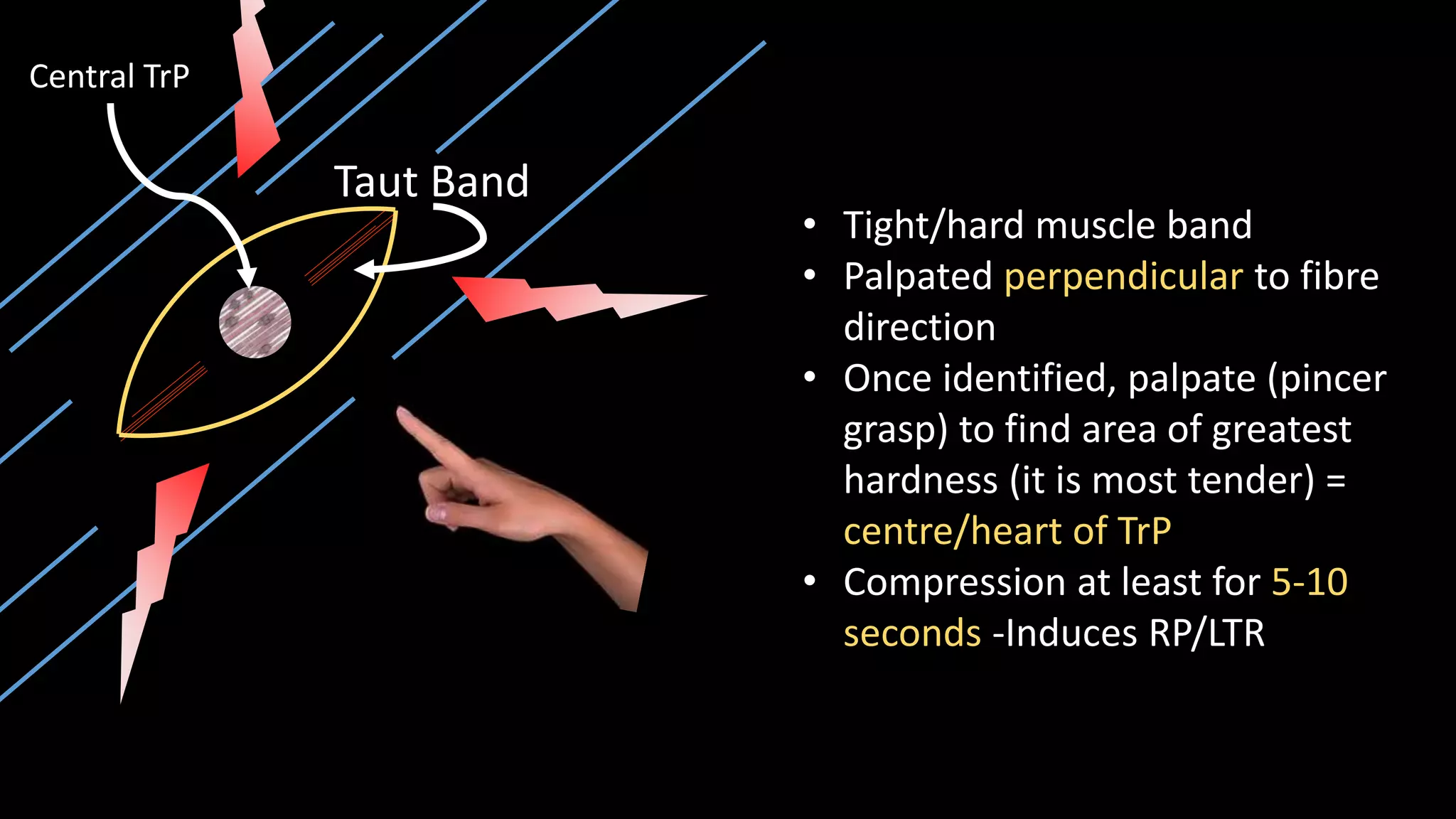
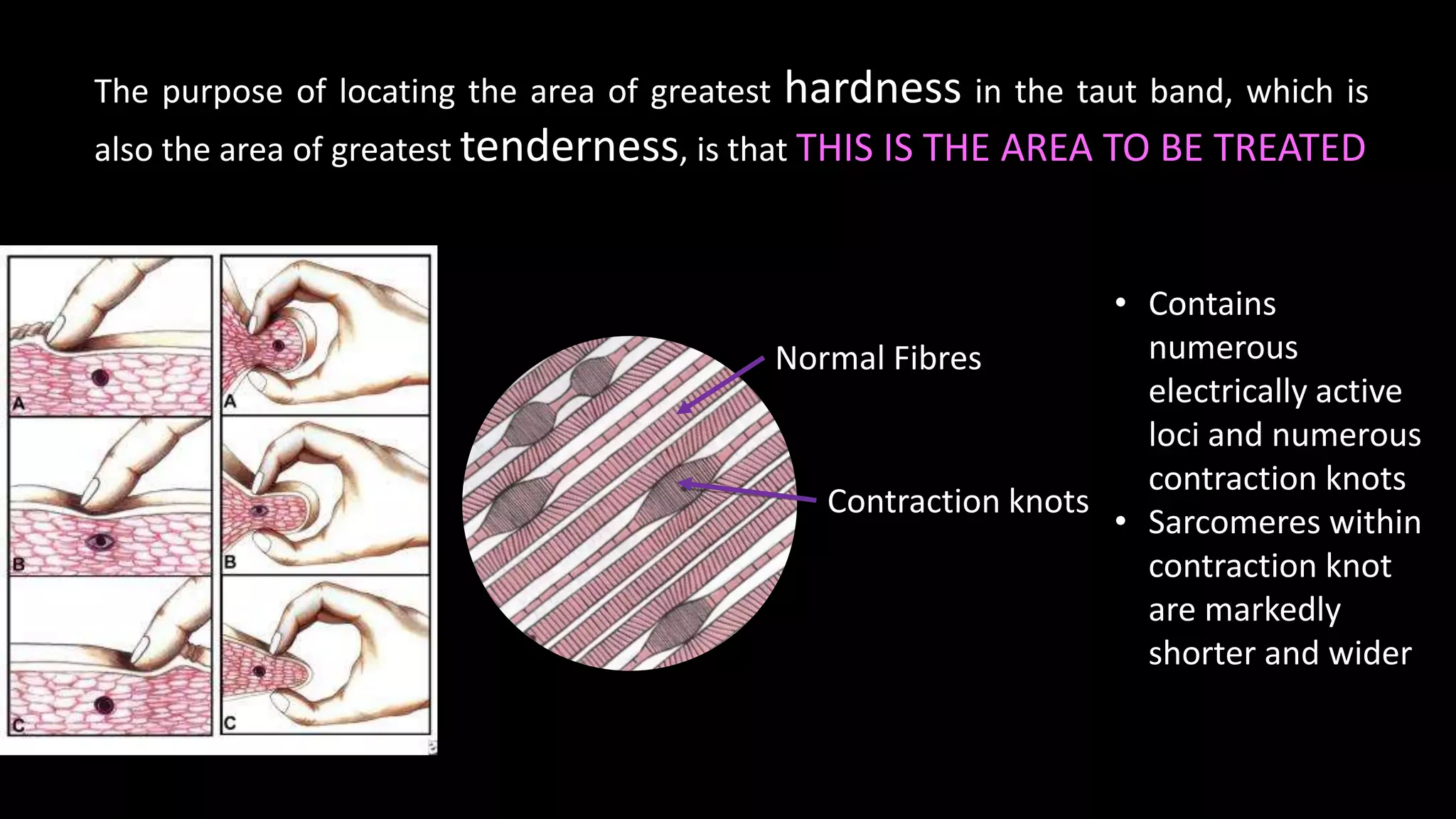
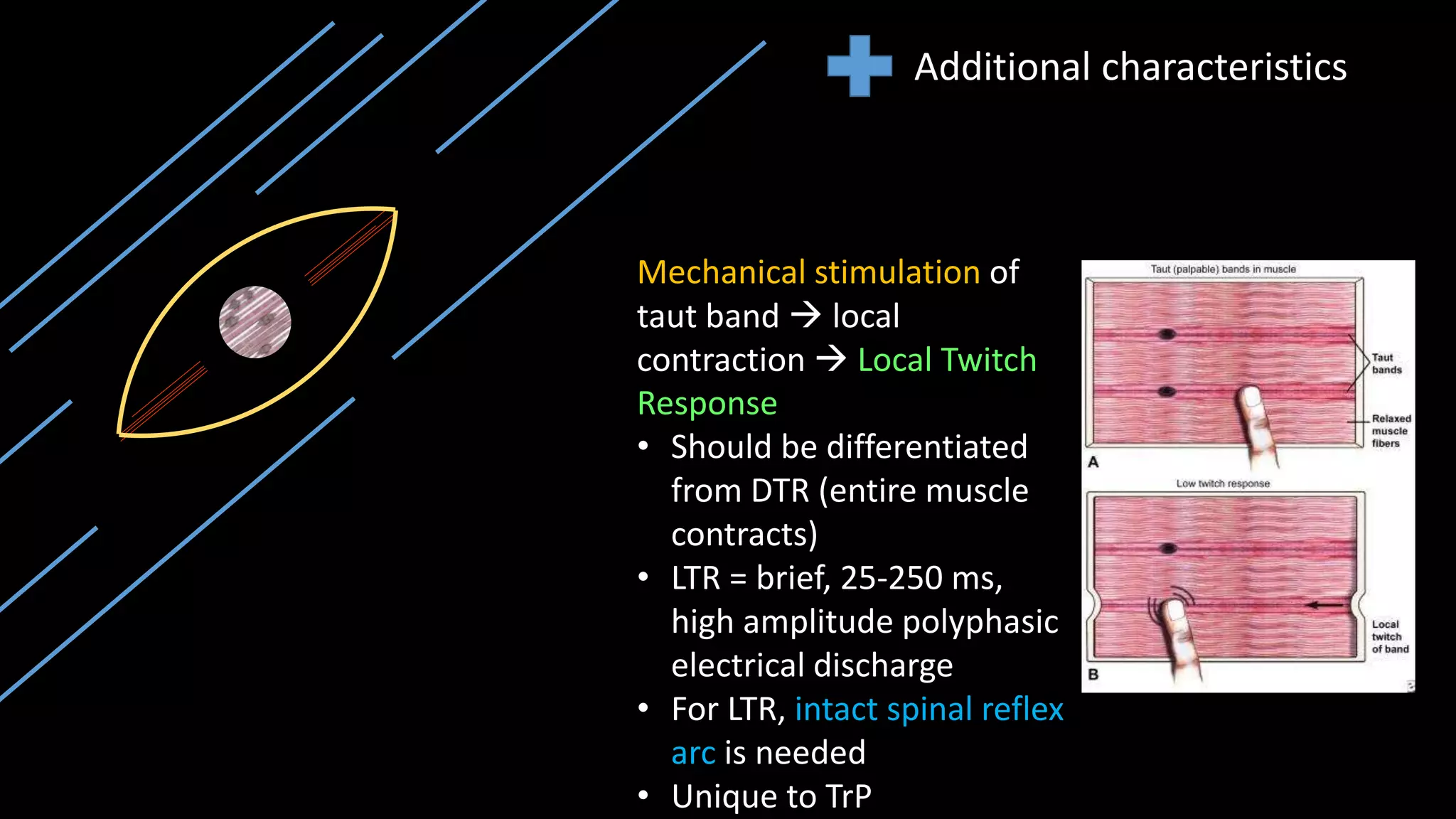
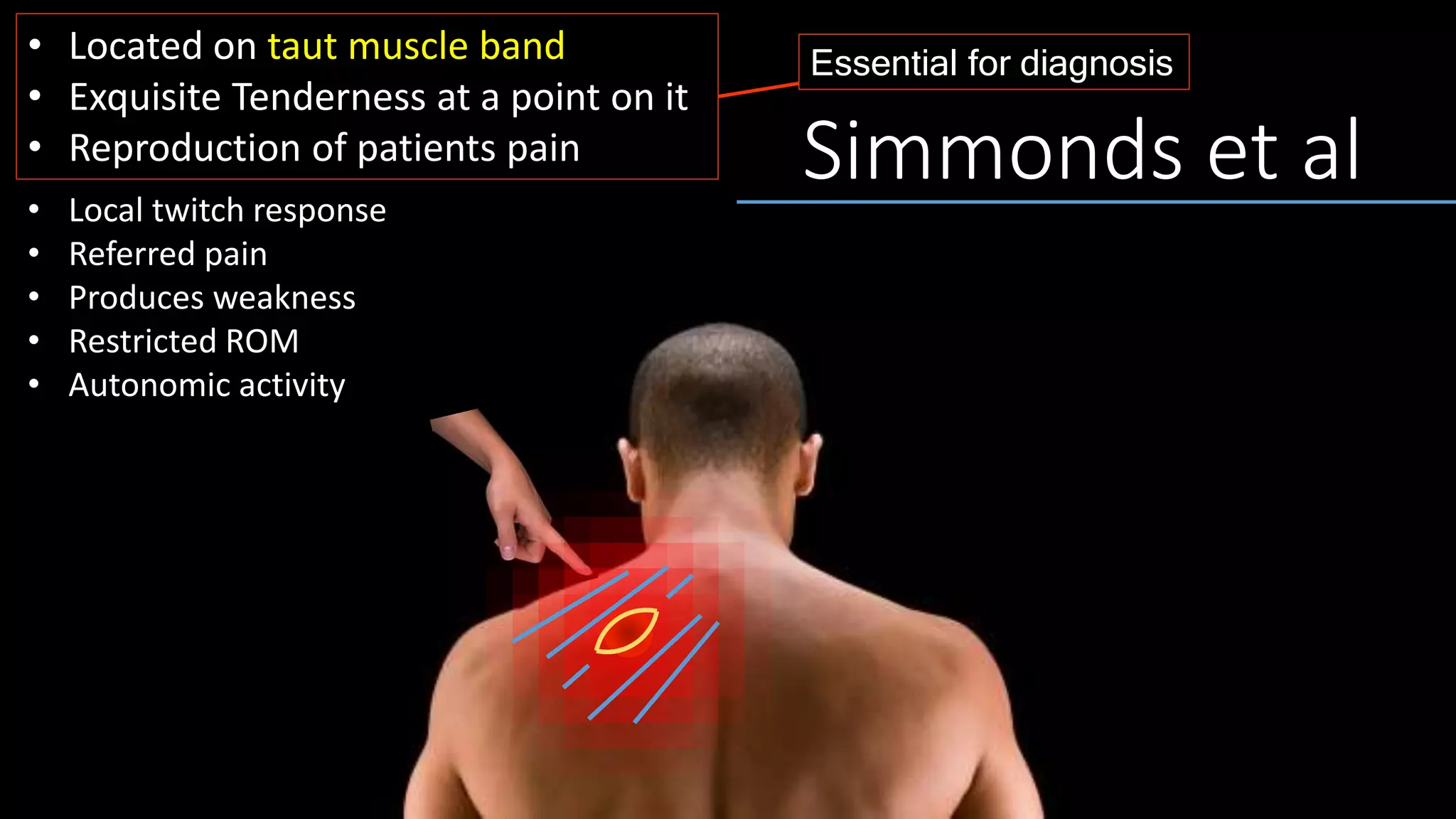
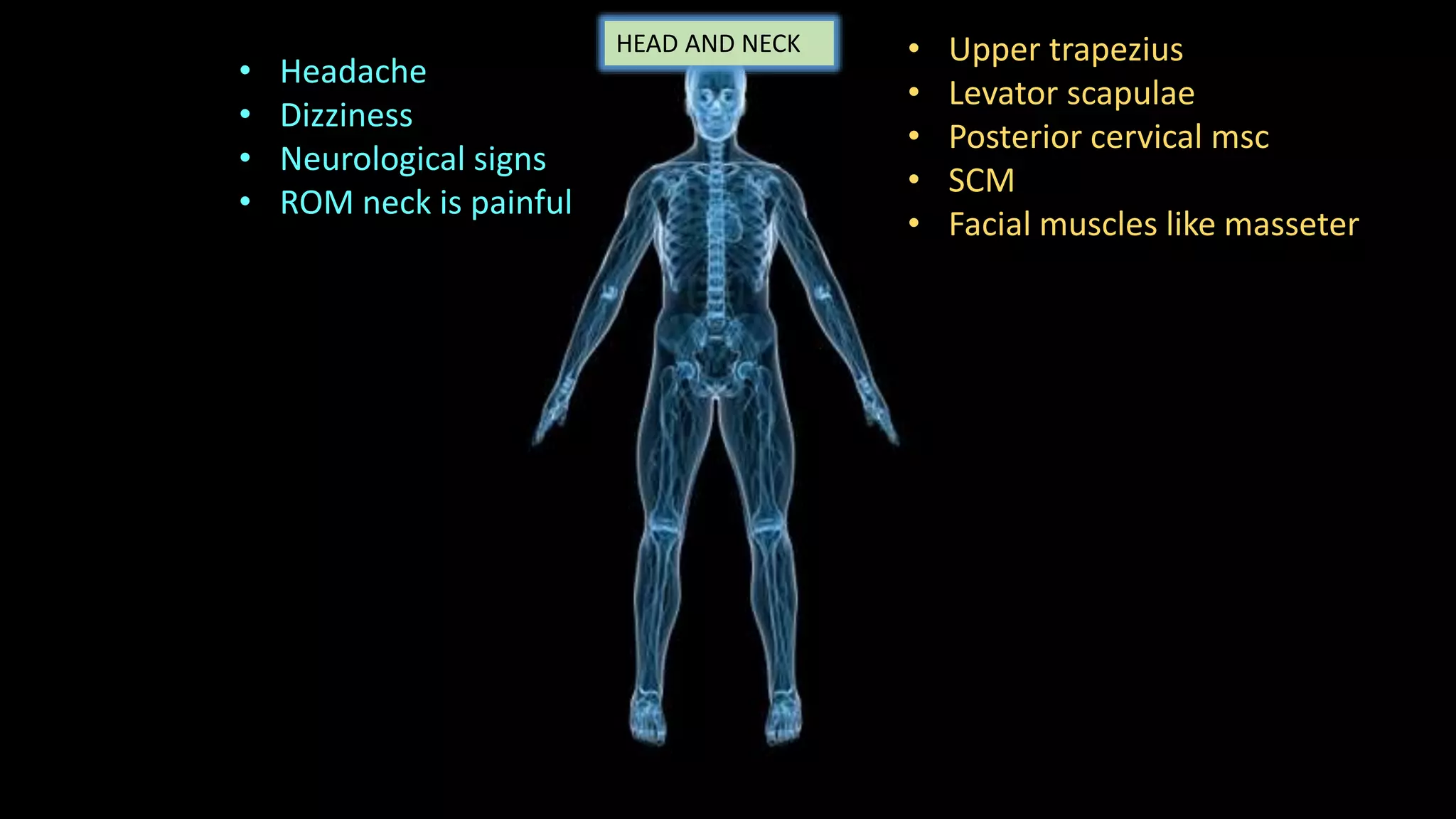
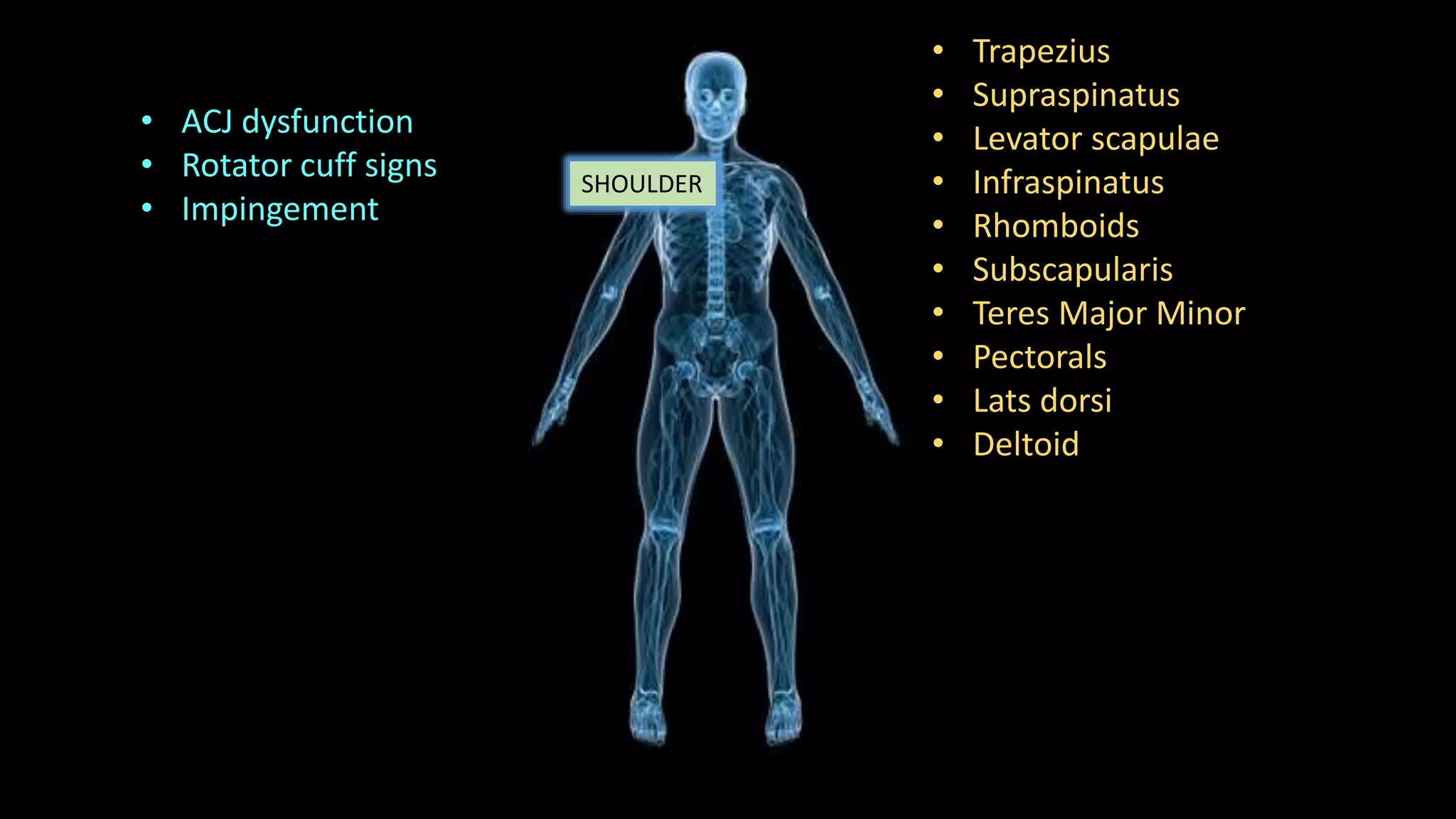
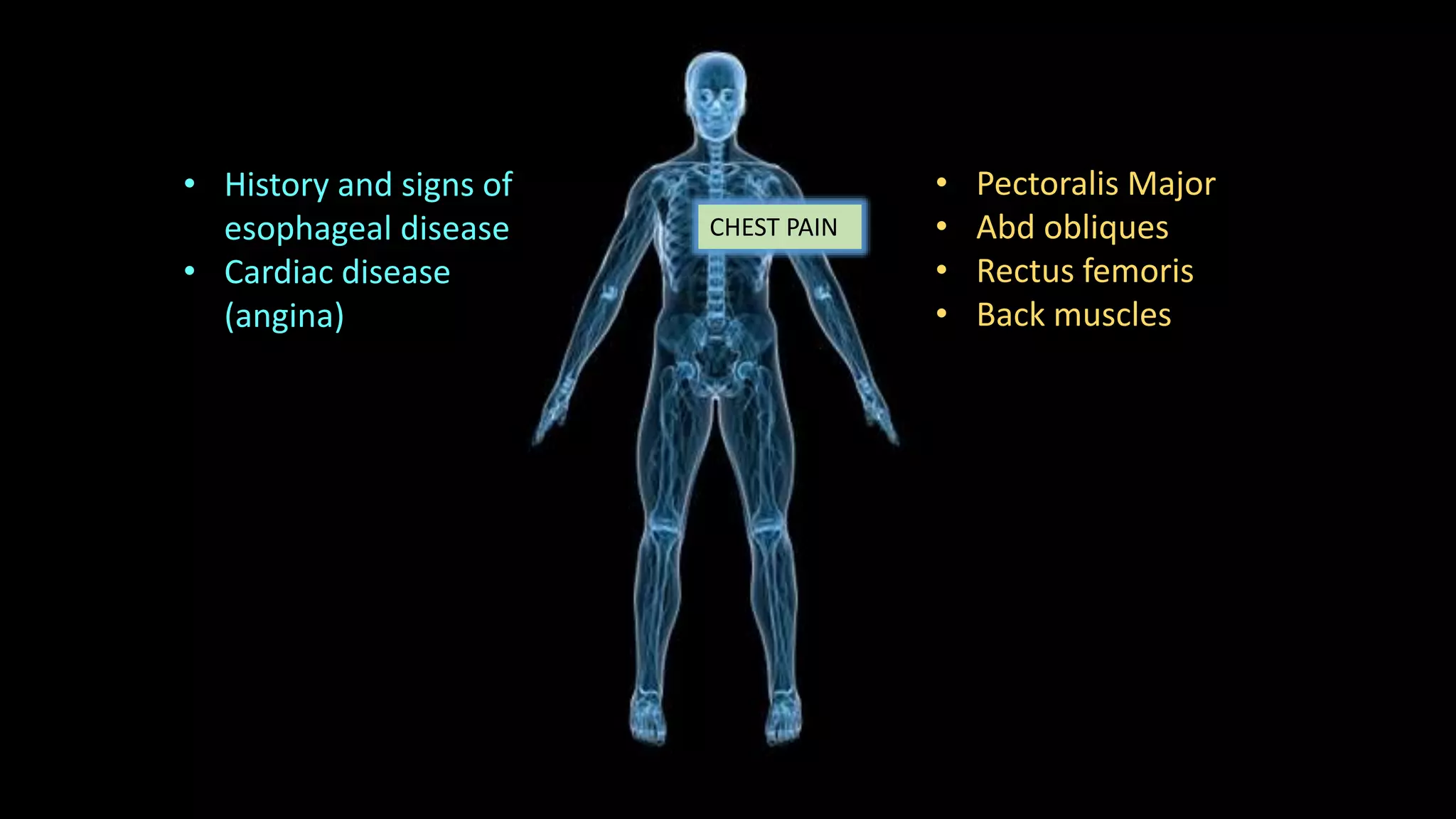
Myofascial pain syndrome is characterized by painful muscle trigger points that cause pain in the affected muscle and potentially other referred pain in distant areas. Trigger points form due to muscle injury or overuse and maintain a contracted knot within the muscle via a positive feedback loop. Examination involves identifying a taut band within the muscle and locating the most tender point, which may elicit a local twitch response when pressed. Diagnosis is based on identifying a trigger point and reproducing the patient's pain. Treatment involves education, medications, and non-pharmacological therapies like exercise, massage, and dry needling of trigger points.