Obstructive Sleep Apnea
- 1. OBSTRUCTIVE SLEEP APNOEA DEFINATION PATHOPHYSIOLOGY SYMPTOMS DIAGNOSIS MANAGEMENT MCQS DR. SANGAY C. LEPCHA 3RD YEAR ENT RESIDENT
- 2. DEFINATION Intermittent complete collapse of the pharyngeal airway, followed by brief arousals and awakenings which then enable return of the normal breathing. repetitive upper airway obstruction, cardiovascular stimulation and oxygen denaturation in sleep. APNOEA- absence of breathing for at least 10 seconds HYPOPNEA- 30% reduction in breathing amplitude with at least 3 % oxygen desaturation or Respiratory related arousal(RERA) via EEG or nasal limitation pattern.
- 3. OBSTRUCTIVE SLEEP APNOEA/HYPOPNEA SYNDROME Comprises of more than 5 obstructed breath/hour and Excessive daytime sleepiness not better explained by other factors Or 2 or more of the following Choking or gasping in sleep Recurrent awakenings Unrefreshed sleep Daytime fatigue Impaired concentration
- 4. UPPER AIRWAY RESISTANCE SYNDROME Patients have symptoms of OSA and polysomnography evidence of sleep disturbance but have minimal obstructive apneas and hypopneas and do not exhibit oxyhemoglobin desaturation
- 5. Grading of obstructive sleep apnoea According to the apnoea-hypopnoea index(AHI) AHI<5 – Normal AHI 5-15- Mild OSA AHI 16-30- Moderate OSA AHI >30- Severe OSA
- 6. PATIENTS OF SLEEP DISORDERED BREATHING OSCILLATES BETWEEN SPECTRUM OF SIMPLE SNORING TO CHRONIC HEAVY SNORING UPPER AIRWAY RESISTANT SYNDROME MILD OSA MODERATE OSA,SEVERE OSA OBESITY HYPOVENTILATION SYNDROME
- 7. PATHOPHYSIOLOGY ADULTS: Intermittent hypoxia ---->sympathetic stimulation------->insulin resistance and metabolic disturbances--------> release of inflammatory cytokine/free radicals---- ----> vascular endothelial derived growth factor, free radicals--------->vascular remodelling--------> atherosclerosis, cardiovascular disease, cerebrovascular accidents , diabetes mellitus, organ and tissue dysfunction. CHILDRENS: Adeno tonsillar hypertrophy------->airway obstruction worsens Obesity----->airway obstruction------->oropharyngeal crowding by excess adipose tissues. Inflammatory markers CRP increases -------> oxidative stress ------>atherogenesis- ----> cardiovascular features----->left ventricular diastolic dysfunction.
- 8. SYMPTOMS( adults) Day time symptoms Excessive day time sleepiness Morning headaches Neurocognitive impairment- secondary impact on memory and learning ,executive functioning and motor coordination Diminished quality of life Mood and personality changes Sexual dysfunction Nocturnal symptoms Snoring Witnessed apneas Choking /gasping Dry mouth Bruxism Restless sleep/frequent arousal Gastroesophageal reflux nocturia
- 9. Symptoms (children) Day time symptoms Mouth breathing Halitosis Behavioral and neurocognitive disorder Impaired growth Nocturnal symptoms Snoring Sleep pauses Breath holding Gasping Perspiration Bed wetting Unusual sleep position
- 10. EXAMINATION OF PATIENT WITH OSA HISTORY TAKING- BETTER IF PATIENTS PARTNER IS AROUND Clinical Examination- BMI(>28mg/m square) high risk of OSA Neck collar size measurement - >17inches Cranial or facial skeletal framework- look for micrognathia, maxillary retrusion ,presence or absence of retrognathia. Detailed nasal and oropharyngeal examination – external nasal deformity, abnormal nasal valve function, deviated nasal septum, nasal polyps, limitation of mouth opening, laxity of soft palate ,size of tonsils, length of the uvula, general crowdedness of the teeth, Mallampati palate position.
- 11. Subjective questionnaires –( ASSESSMENT OF EXCESSIVE DAY TIME SLEEPINESS) Epworth Sleepiness Scale (ESS)( score of more than 10 out of 24 may indicate ESS) Stop Bang questionnaire( score more than 5 than there is high risk of OSA) Objective questionnaires- Multiple sleep latency test(<8 min) Maintanence of wakefulness test
- 12. EPWORTH SLEEPINESS SCALE SITUATION 1. Sitting and reading 2. Watching tv 3. Sitting inactive in public places 4. As a passenger in car for an hour without a break 5. Lying down in the afternoon when the circumstances permit 6. Sitting and talking to someone 7. Sitting quietly after a lunch without alcohol 8. In a car, while stopped for a few minutes in traffic
- 13. STOP BANG QUESTIONNAIRE 1. Snoring 2. Tired 3. Observed 4. Blood pressure 5. BMI 6. Age 7. Neck circumference 8. gender
- 14. In childrens- look for Syndromic child- Downs syndrome, Treacher Collins syndrome, CHARGE syndrome Pierre robin syndrome Obesity Sickle cell disease asthma
- 15. INVESTIGATIONS Single channel- overnight oximetry Multichannel- respiratory and oximetry In hospital full polysomnography- respiratory, oximetry and sleep architecture assessment using electroencephalography, electrooculography and electromyography parameters CT scans and MRI Sleep nasendoscopy Multichannel pressure measurements
- 16. Overnight oximetry Pulse oximeter applied at the end of a digit which is attached to a wrist watch computer that the patient wears at night. Measures variation of pulse and oxygen saturation during sleep. Based of the principle that during apnoea and hypopnoea there is fall in oxygen saturation which is known as “oxygen dips” Indicators Dip of 4% oxygen saturation (94% to 90%) than a 2% or 3% dip Oxygen desaturation index(ODI) - >15/hour
- 17. Additional features- ESS >10 BMI>28mg/square metre comorbidities (hypertension, coronary artery disease, metabolic syndrome and diabetes mellitus) Important pointers ODI >15 can be used only when patients resting oxygen saturation is more than 90 and in absence of obstructive lung disease.
- 18. Multichannel testing Nasal /oral flow measured via pressure cannula Abdominal movements via pressure transducer in house velcrobelt Pulse oximetry
- 19. polysomnography Hospital based Utilises Electroencephalography, electrooculography, electromyography snoring microphone ECG Nasal /oral airflow Thoracic effort, abdominal effort Pulse oximetry
- 20. Sleep nasendoscopy Allows three dimensional visualization of the upper airway dynamics during sleep Drug induced Operation theatre, anaesthetist, adequate cardiovascular and respiratory monitoring. Controversies : drug induced sleep different from the physiological sleep Exaggeration of the muscle relaxation Depth of the anaesthesia
- 21. Multichannel pressure transducers Pressure catheters Measures pressure at various anatomical location between nasopharynx to oesophagus Disadvantage- possibility of some movement of catheter at different phase of respiration.
- 22. Management of OSA NON SURGICAL MANAGEMENT: Lifestyle modification- reduction of weight Avoidance of alcohol and smoking Regular exercise Positional therapy- avoidance of supine position while sleeping.
- 23. MANDIBULAR ADVANCEMENT SPLINTS Produces forward displacement of the mandible thereby bringing the tongue base anteriorly increases dimensions of upper airway. TONGUE RETAINING DEVICES Side effects- Excessive salivation Temporomandibular joint pain and bite change
- 24. Medical management Continuous positive airway pressure(CPAP) PRINCIPLE: “pneumatic splint” air pressure is generated by a tube or a mask through oral or nasal passage which prevents collapse of pharyngeal or palatal walls thereby maintaining airway. Types- fixed pressure auto-CPAP Calculating the pressure required- 1)Mathematical equation (0.16 x BMI) + (0.13 X NC) + (0.04 X AHI) -5.12 2)Overnight Polysomnography – 1st half diagnosing OSA and 2nd half for titrating CPAP
- 25. Compliance- usage of CPAP for more than 4 hours for at least 5 nights per week. Side effects- Claustrophobia Nasal stuffiness Skin abrasion and leaks Air swallowing Barotrauma
- 26. ALTERNATIVE TO CPAP Bilevel positive airway pressure( BiPAP) Allows specific pre –set inspiratory(10 -20 cm of H2O) and expiratory pressure(5 - 10 cm of H2O)
- 27. Surgical management of OSA INDICATIONS: Apnoea/ hypopnoea index ≥20 events/ hour Oxygen desaturation <90% Esophageal pressure more negative than -10 mm hg Cardiovascular derangements (arrythmia, hypertension) Neurobehavioral symptoms(excessive day time sleepiness) Failure of medical management Anatomical sites of obstruction CONTRAINDICATIONS: Severe pulmonary disease Unstable cardiovascular disease Morbid obesity Alcohol or drug abuse Psychiatry unstability
- 28. 1) NASAL SURGERY Indications- significant nasal obstruction secondary to deviated nasal septum, nasal polyps, nasal valve collapse. Rationale – improvement of nasal airway thereby increases compliance with CPAP.
- 29. 2)UVULOPALATOPHARYNGOPLASTY INDICATIONS: Posterior nasal spine to uvula distance >38mm Tonsil size – grade 3 and 4 b/l Posterior airway space >10mm Friedman tongue position 1 or 2 Absence of retrognathia, retroglossia, lateral pharyngeal wall bulging, morbid obesity.
- 30. Removal of 1- 2cm of the oral palatal mucosa curvilinear fashion along with the anterior pillars excision of excessive length of the soft palate. Nasopharyngeal mucosa pulled anteriorly to widen the airway Side effects- postoperative pain velopharyngeal insufficiency Compromise future use of CPAP.
- 35. Zetapalatopharyngoplasty Goals Removal of anterior pillar Splitting of soft palate in midline
- 37. 3)LASER ASSISTED UVULOPALATOPLASTY CO2 laser used- Nd- YAG laser- Side effect- postoperative pain pharyngeal contracture and stenosis fungal infections haemorrhage temporary loss of taste and palatal incompetence globus type symptom
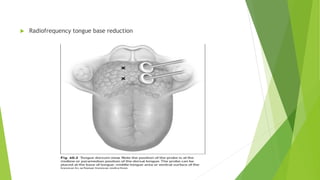
- 39. 4)RADIOFREQUENCY TISSUE VOLUME REDUCTION / THERMAL ABLATION Low frequency radio waves -----> submucosal tissue -----> charged ions------- >denaturation of proteins-------->cell lysis(60-90degree) minimal collateral damage Types – somnus , celon , coblator unit. Advantage- carried out in local anaesthesia.
- 40. Radiofrequency tongue base reduction
- 41. 5)TRANSORAL ROBOTIC SURGERY FOR TONGUE BASE Telerobotic system used, 3d visualization Improved access allows oropharyngeal enlargement anteriorly through tongue base reduction and treatment of floppy epiglottis, arytenoids and aryepiglottic folds
- 42. Lesser performed surgeries Cautery assisted palatal stiffening Snare uvulectomy Injection snoreplasty( doxycycline, ethanol 50%, 3% sodium tetradecyl sulphate) Pillar implants Mandibular and maxillary surgery- genioglossus and tongue base expansion, hyoid suspension, maxillomandibular suspension) Tracheostomy Hypoglossal nerve stimulation
- 43. Surgical management in children Adenotonsillectomy- curettage, electrocautery ablation, coblation Macroglossia and ptotic tongue- Tongue suspension sutures, genioglossus advancement and radiofrequency ablation.
- 44. ALGORITHM FOR MANAGEMENT OF OSA Disease severity Mild (<15 ASI >5) No symtoms-->behavioural modification and consideration of oral appliances, PAP, consider surgical interventions Moderate (<30 AHI>15) No symtoms-->behavioural modification and consideration of oral appliances, PAP, consider surgical interventions Symptoms-->behavioural modifications, PAP, surgical interventions for PAP failures
- 45. Severe symtoms (ASI>30) Symptoms or no symtoms Behavioural modification, PAP, Surgical intervention Consideration of tracheostomy, BMI>40 Bariatric surgeries
- 46. MCQS: 1) AN EPISODE OF SLEEP APNEA IS THE CESSATION OF BREATHING FOR a)10 sec b)20 sec c)30 sec d)40 sec
- 47. 2)False about polysomnography a)Electromyography is done for muscle potential and its activities b)Eye movements are recoded c)Records multiple measures of time taken to sleep d)Continuous EEG recording from the temporal and frontal leads.
- 48. 3) OSA can be associated with the following syndrome except a)Downs syndrome b)Treacher collins syndrome c)CHARGE syndrome d)Turners syndrome
- 49. Indication of uvulopalatopharyngoplasty are all except a)Posterior nasal spine to uvula distance >38mm b)Presence of retrognathia c)Posterior airway space >10mm d)Friedman tongue position 1 or 2
- 50. Select the false statement regarding OSAHS and UARS: a)Seen in both male and female b)OSAHS patients are mostly hypertensives c)Excessive day time sleepiness is seen in both OSAHS and UARS d)Somatic complaints are seen in patients of UARS.