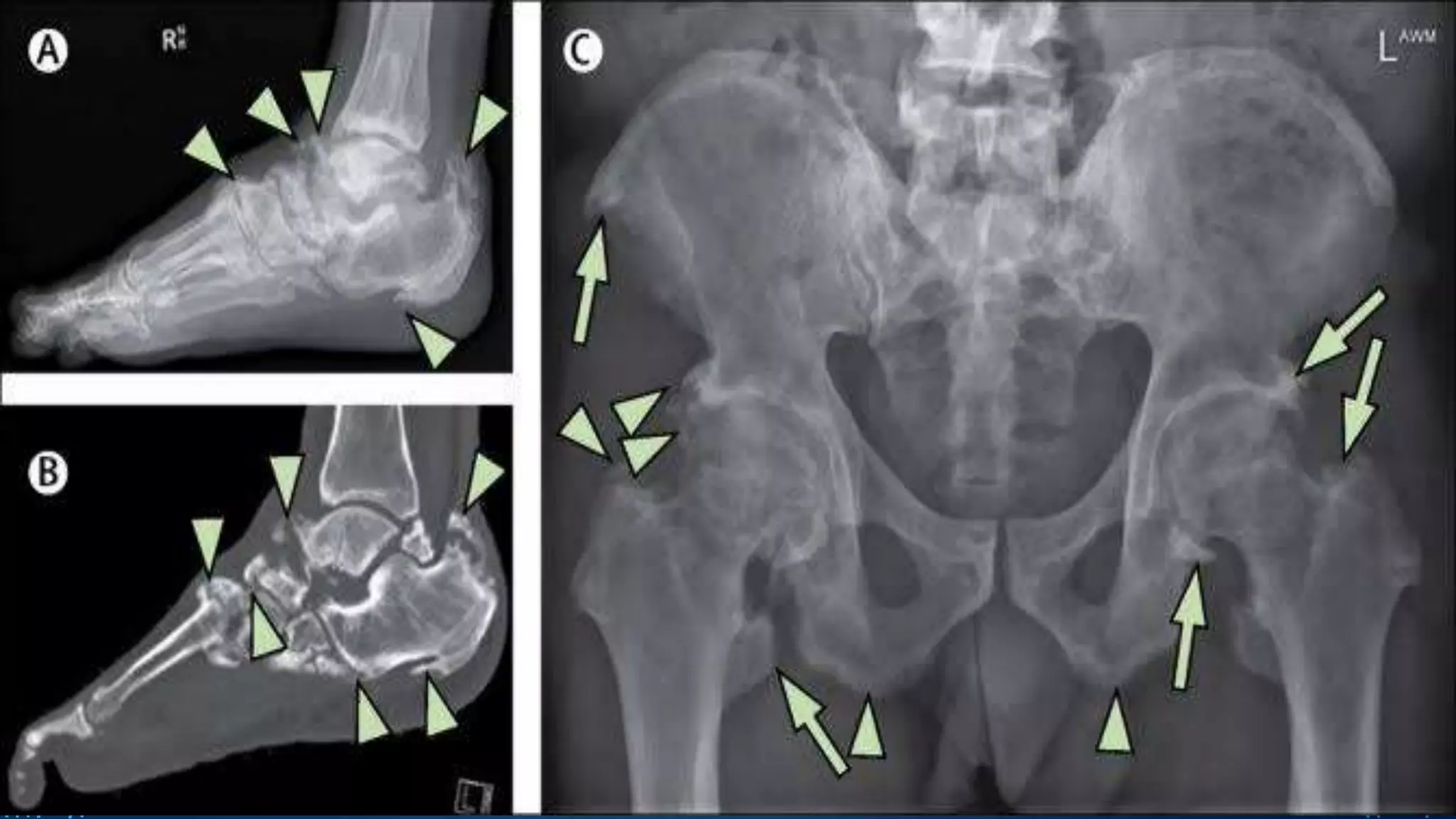
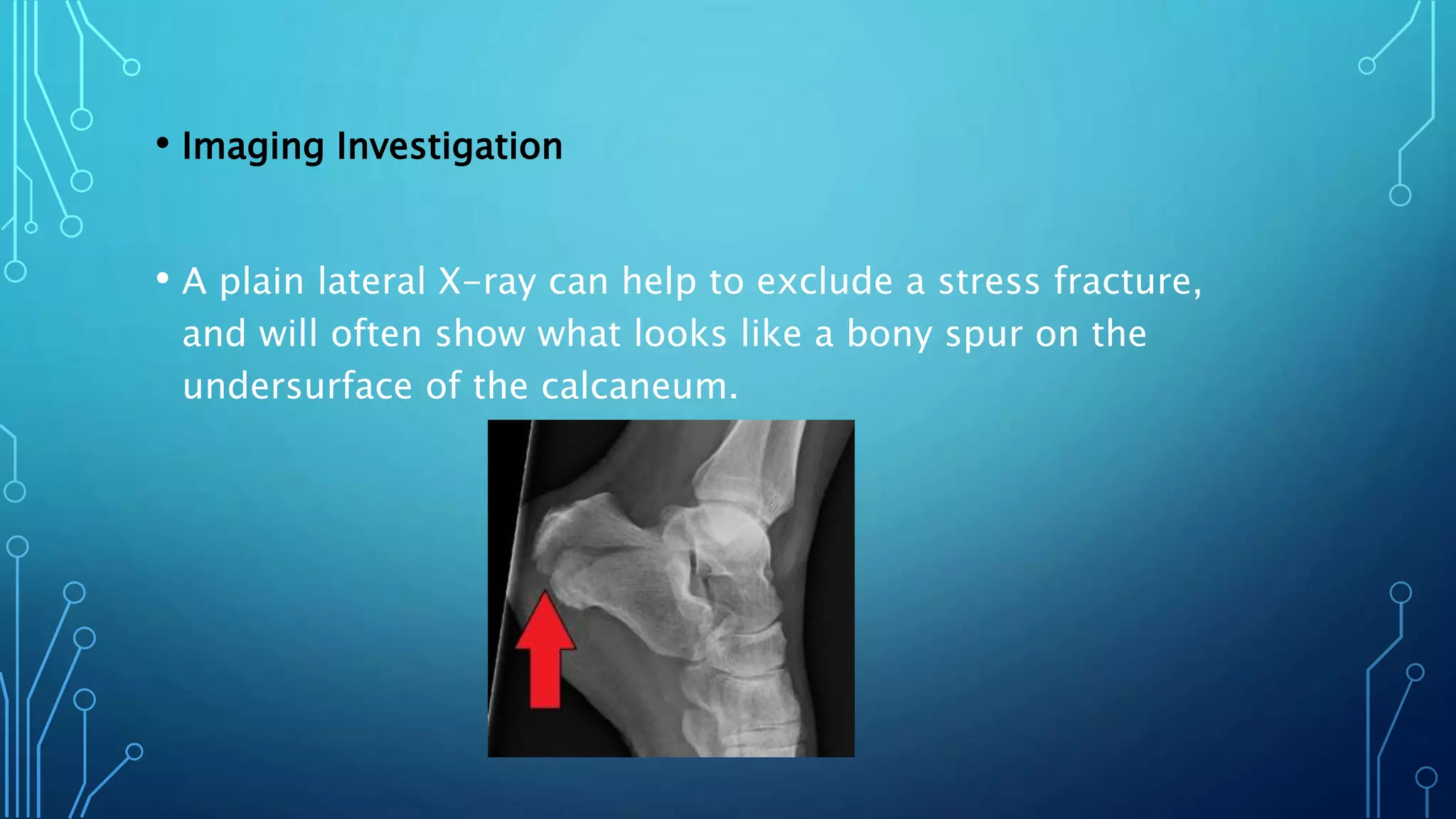
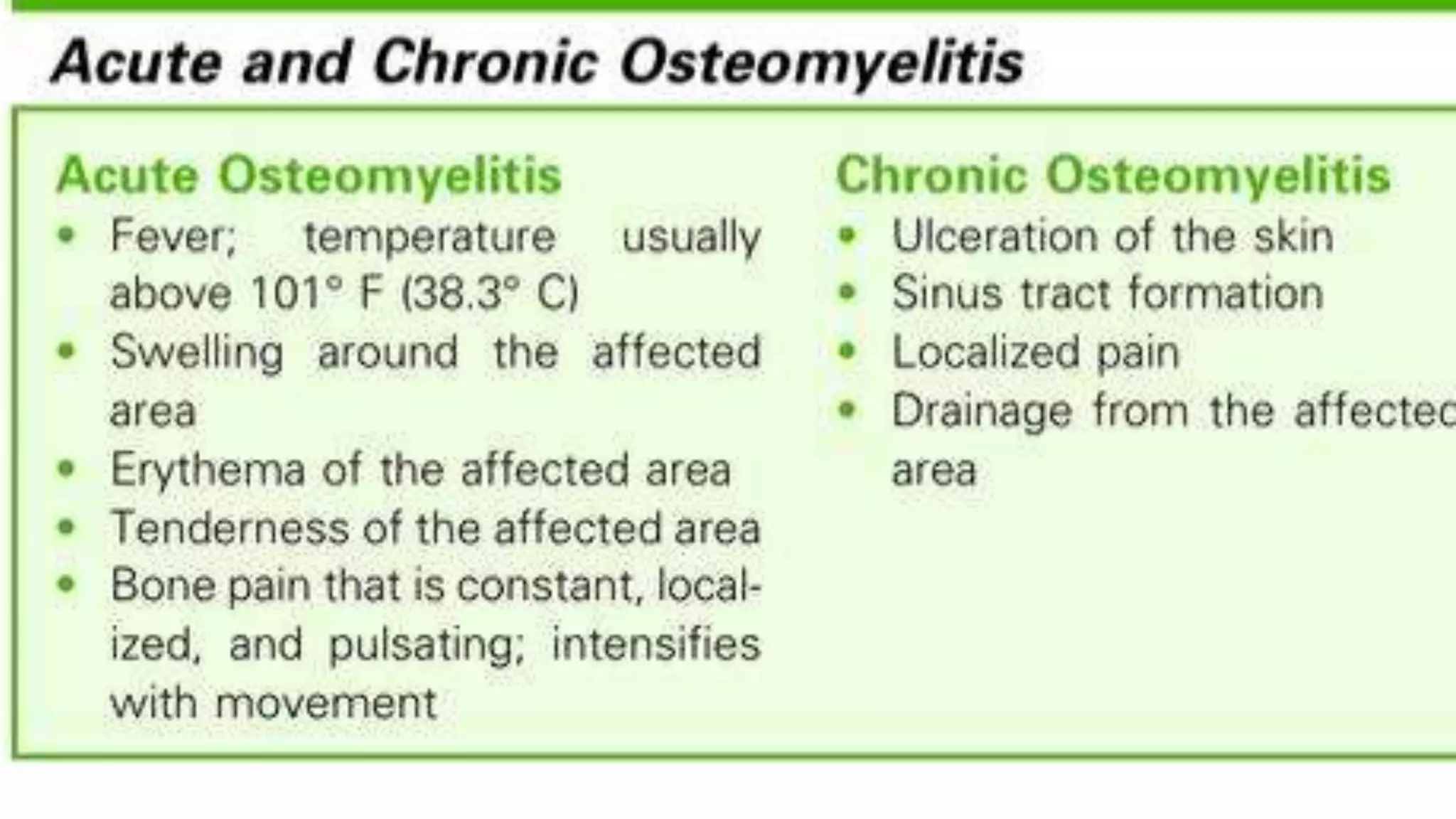
The document discusses various causes of painful heel, including plantar fasciitis, osteomyelitis, arthritis of the subtalar joint, tender heel pad, calcaneal paratendinitis, and post calcaneal bursitis. It describes the pathology, clinical features, differential diagnosis, and treatment options for these conditions. The key points are that plantar fasciitis is the most common cause of pain beneath the heel and tends to improve with rest, stretching, and orthotics over 18-36 months without intervention. Differential diagnosis involves considering trauma, infection or inflammatory diseases as potential underlying causes.