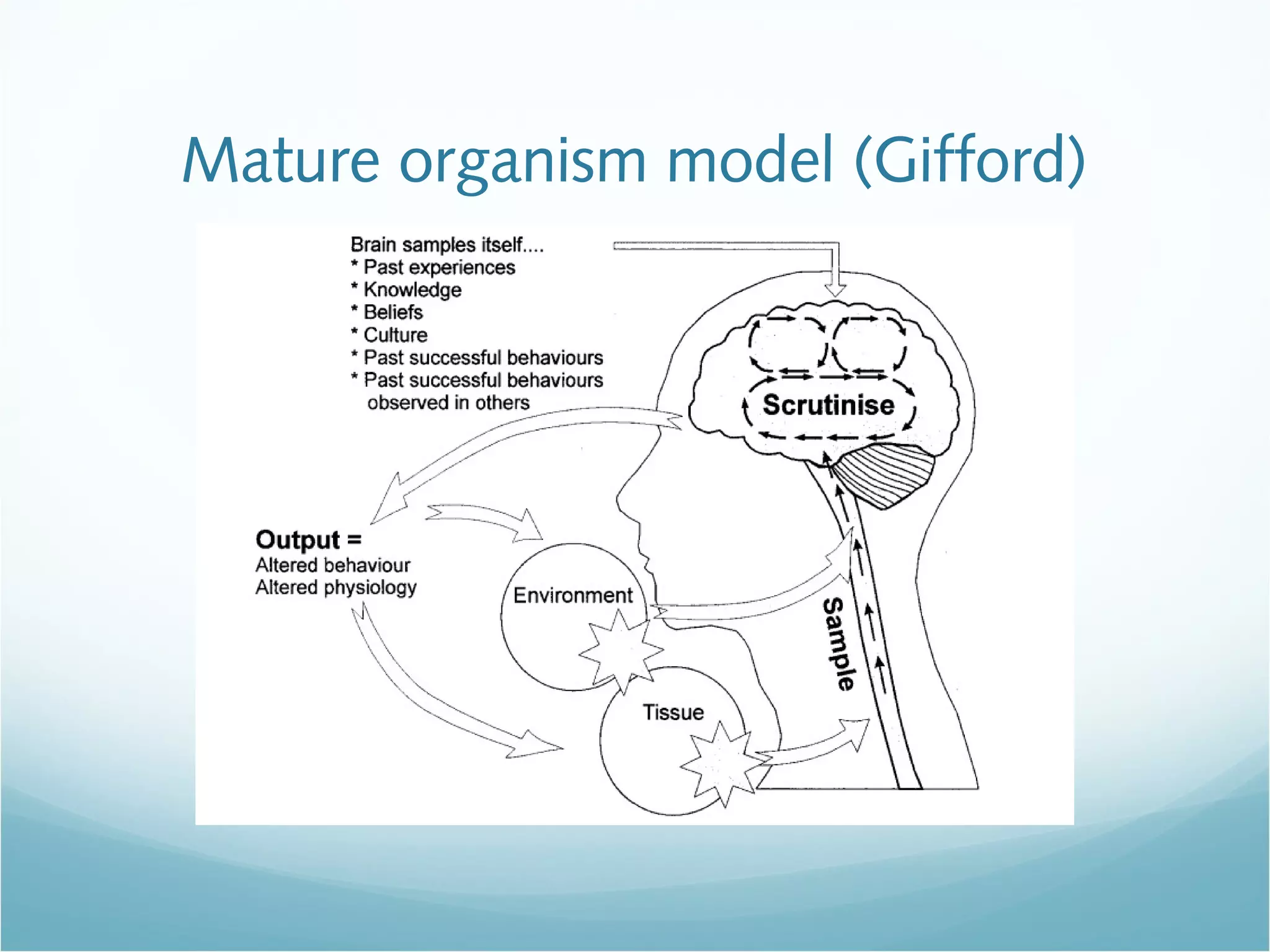
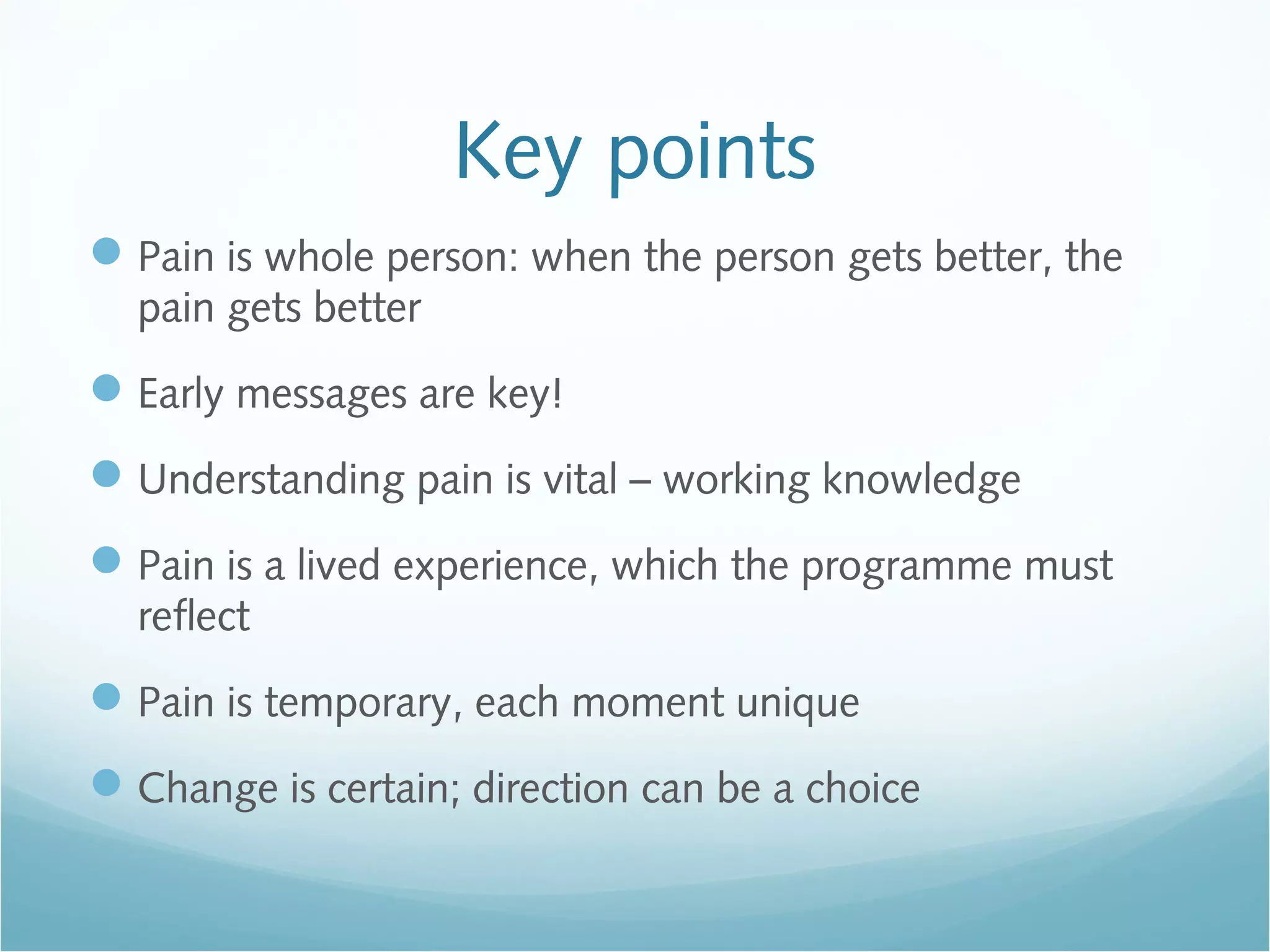
This document discusses pain in the context of sport. It notes that pain is a complex experience influenced by biological and psychological factors. It is not always indicative of actual tissue damage. When an injury occurs, many individual factors like a person's health history, mindset, and early treatment can influence whether the pain persists long-term. Managing persisting pain involves seeing the whole person, understanding pain scientifically, and using rehabilitation to restore normal function and a positive self-identity, rather than just focusing on pain alone.