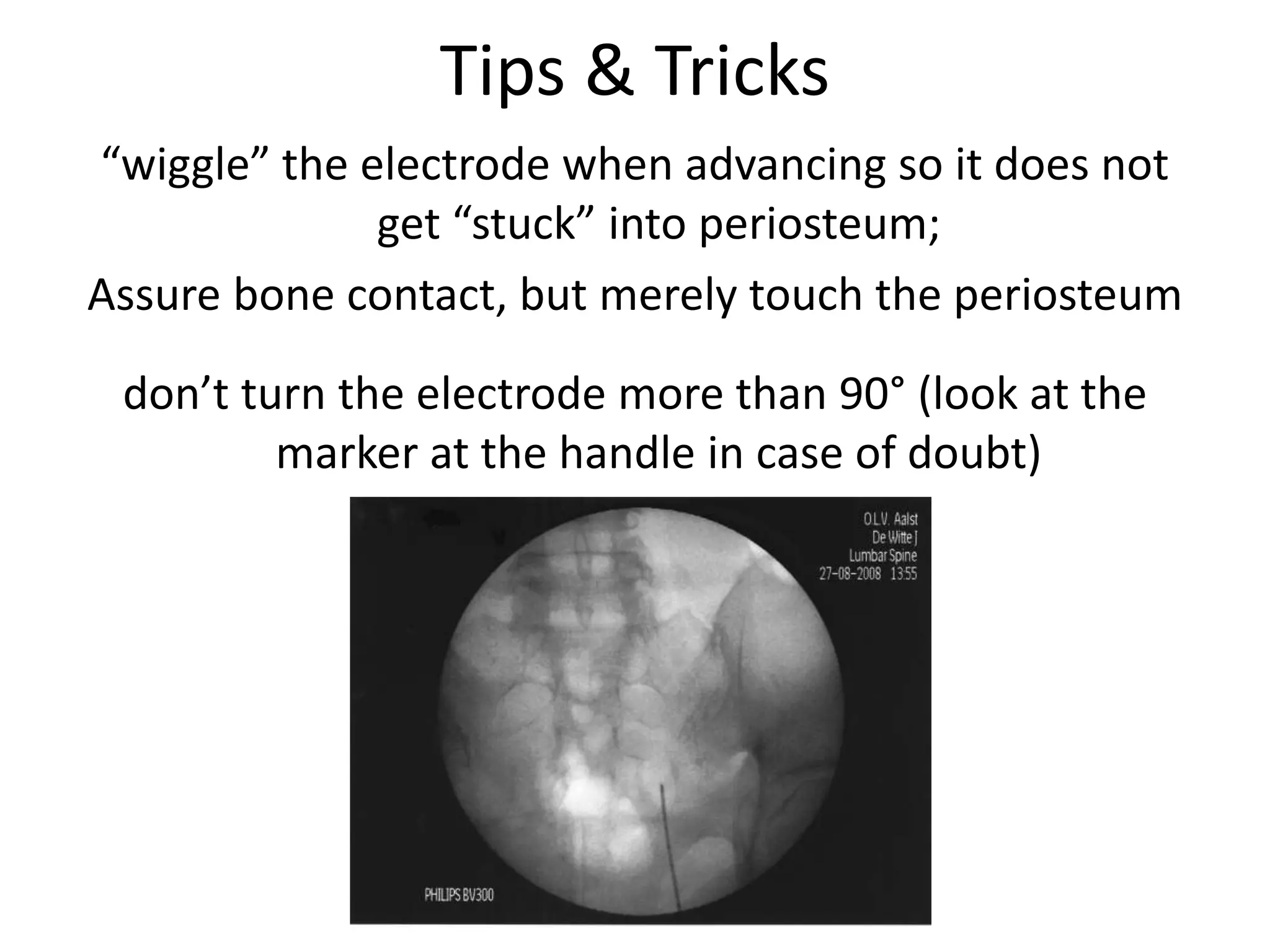
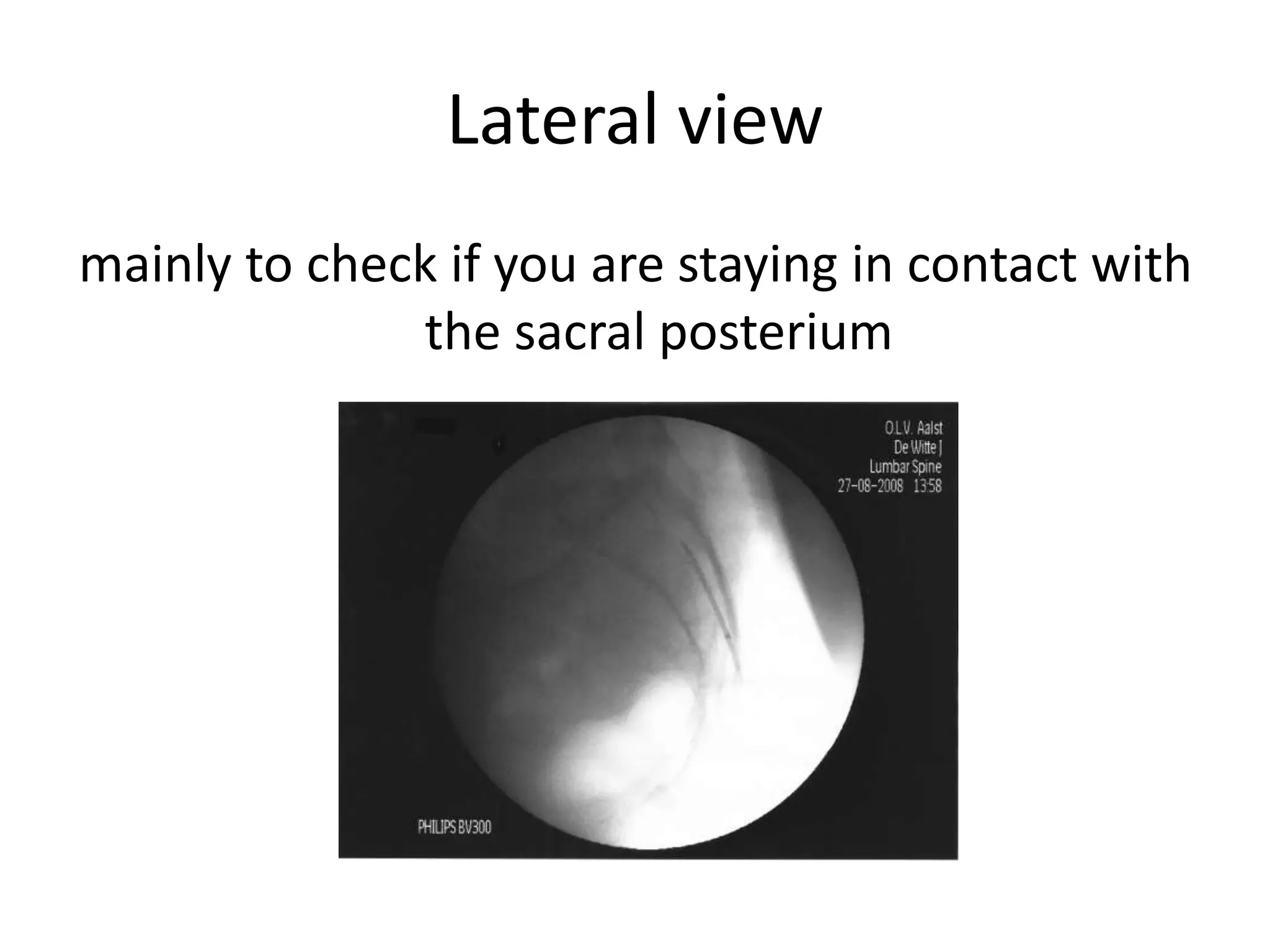
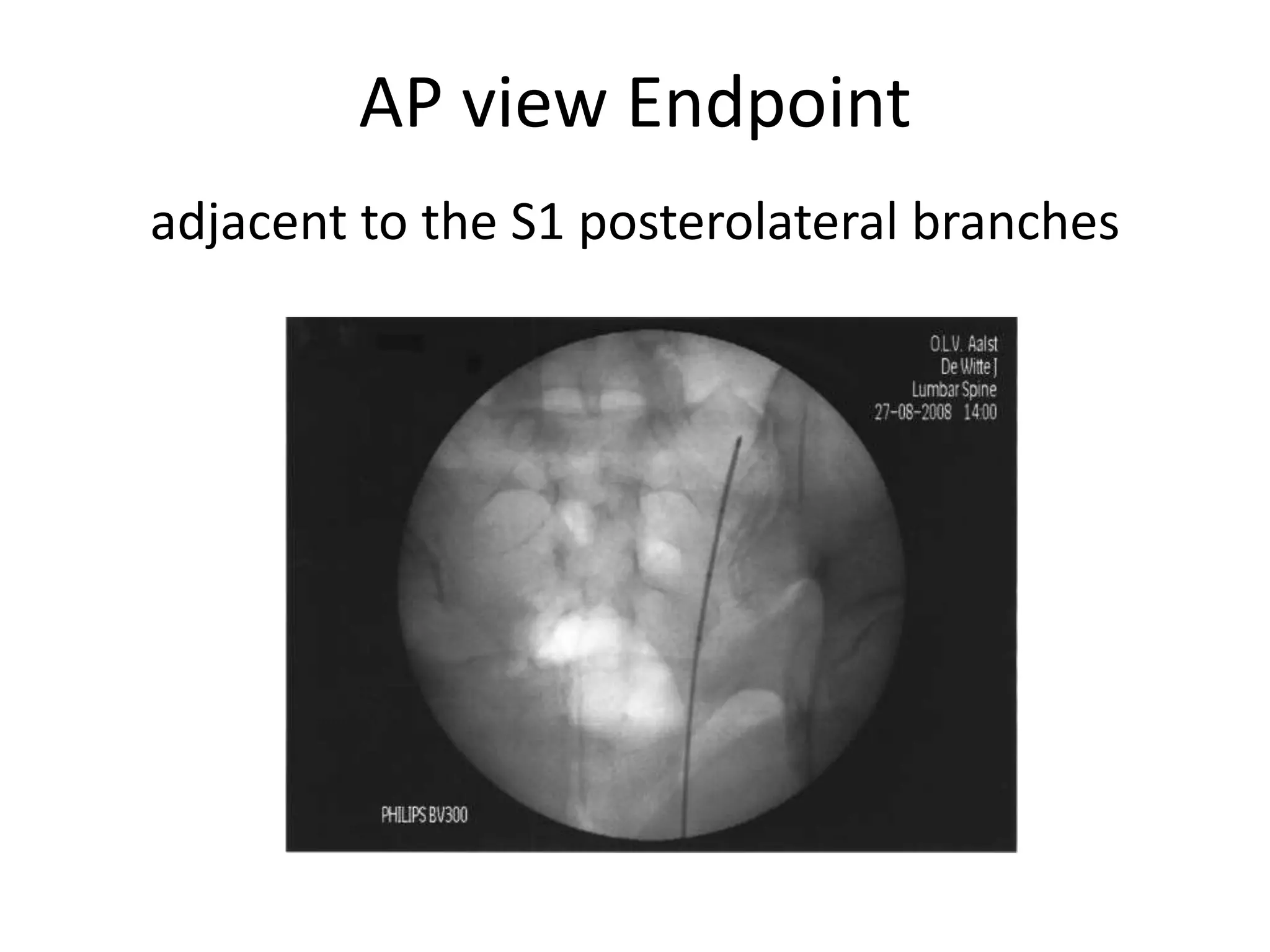
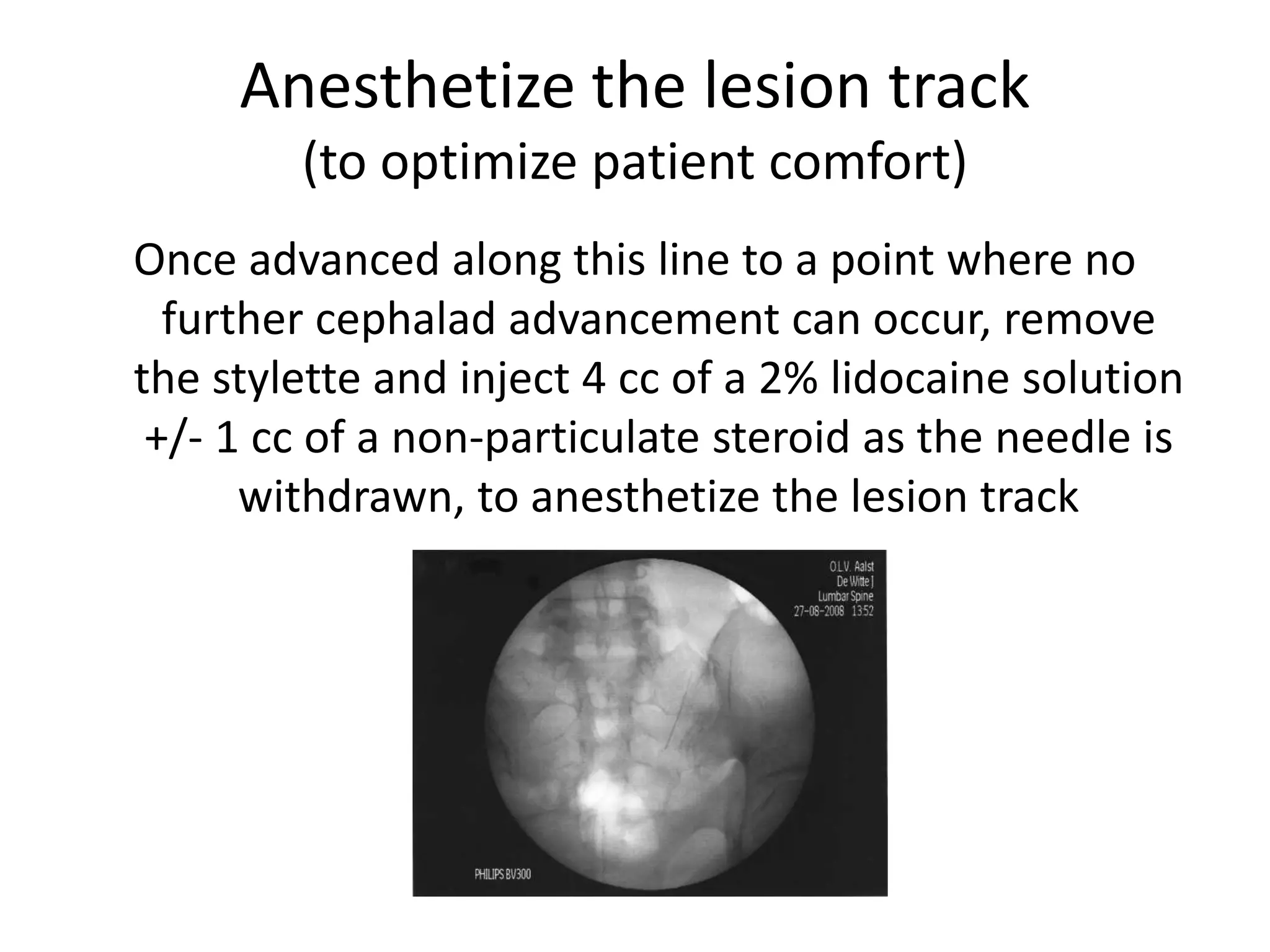
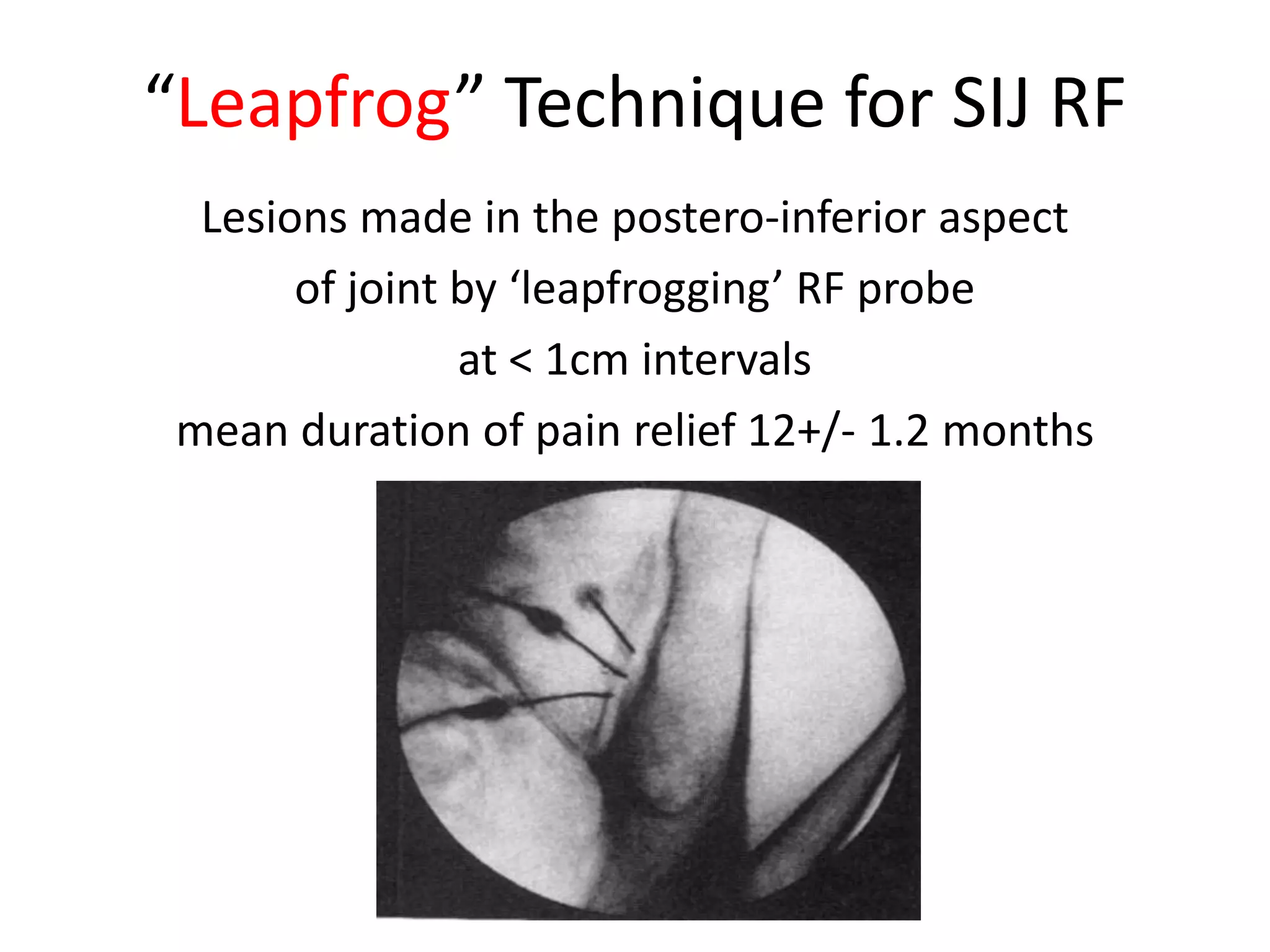
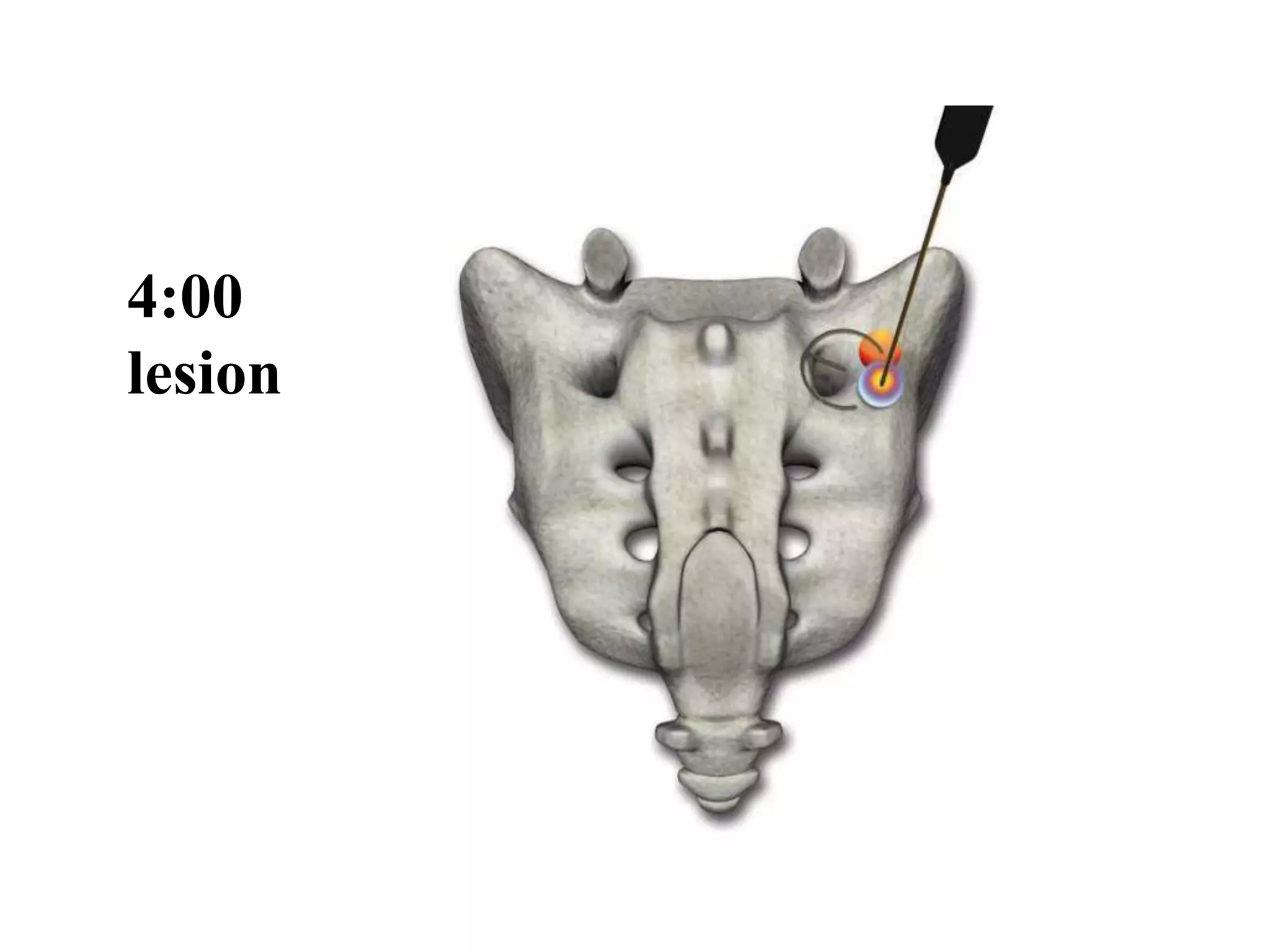
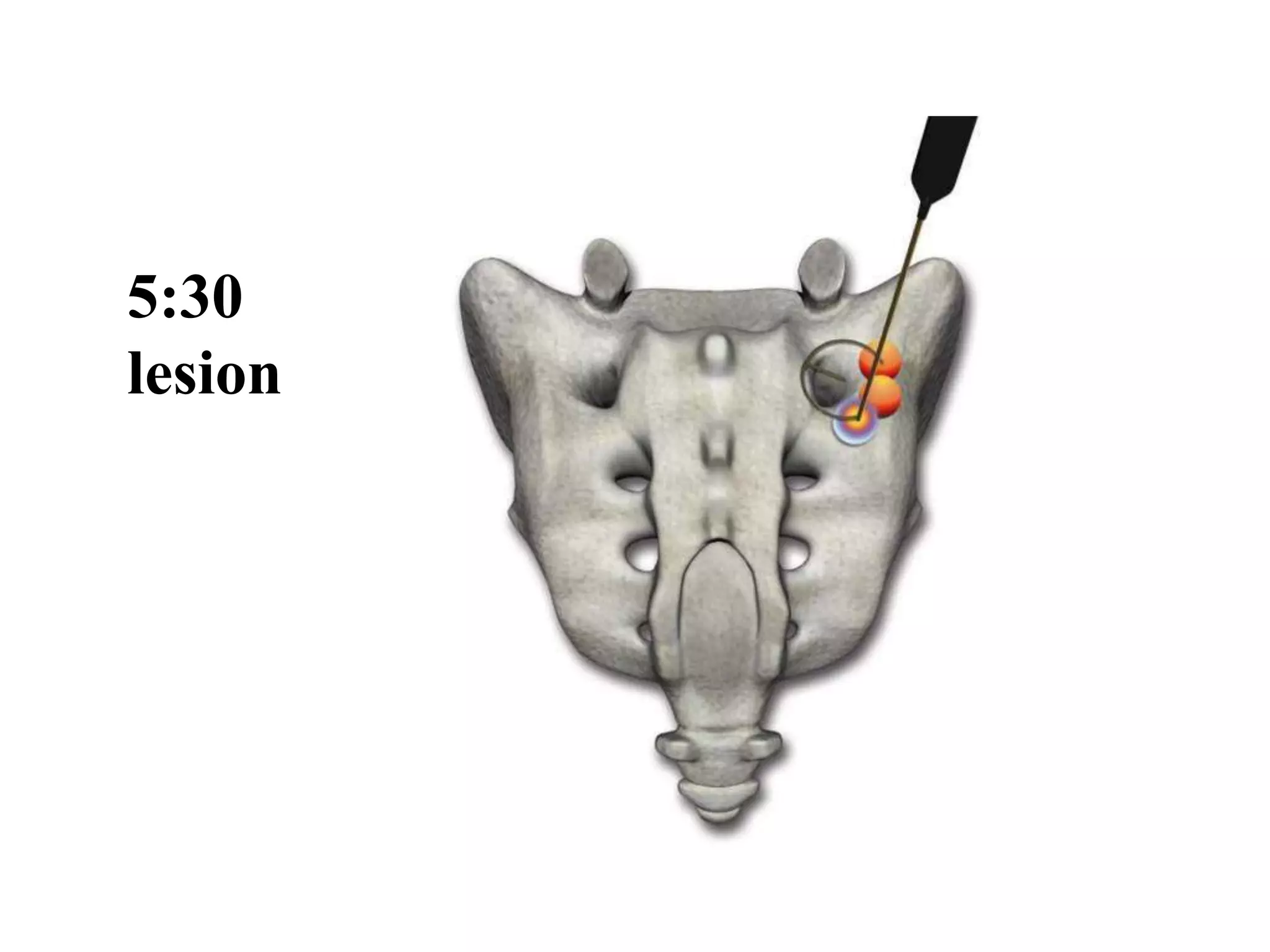
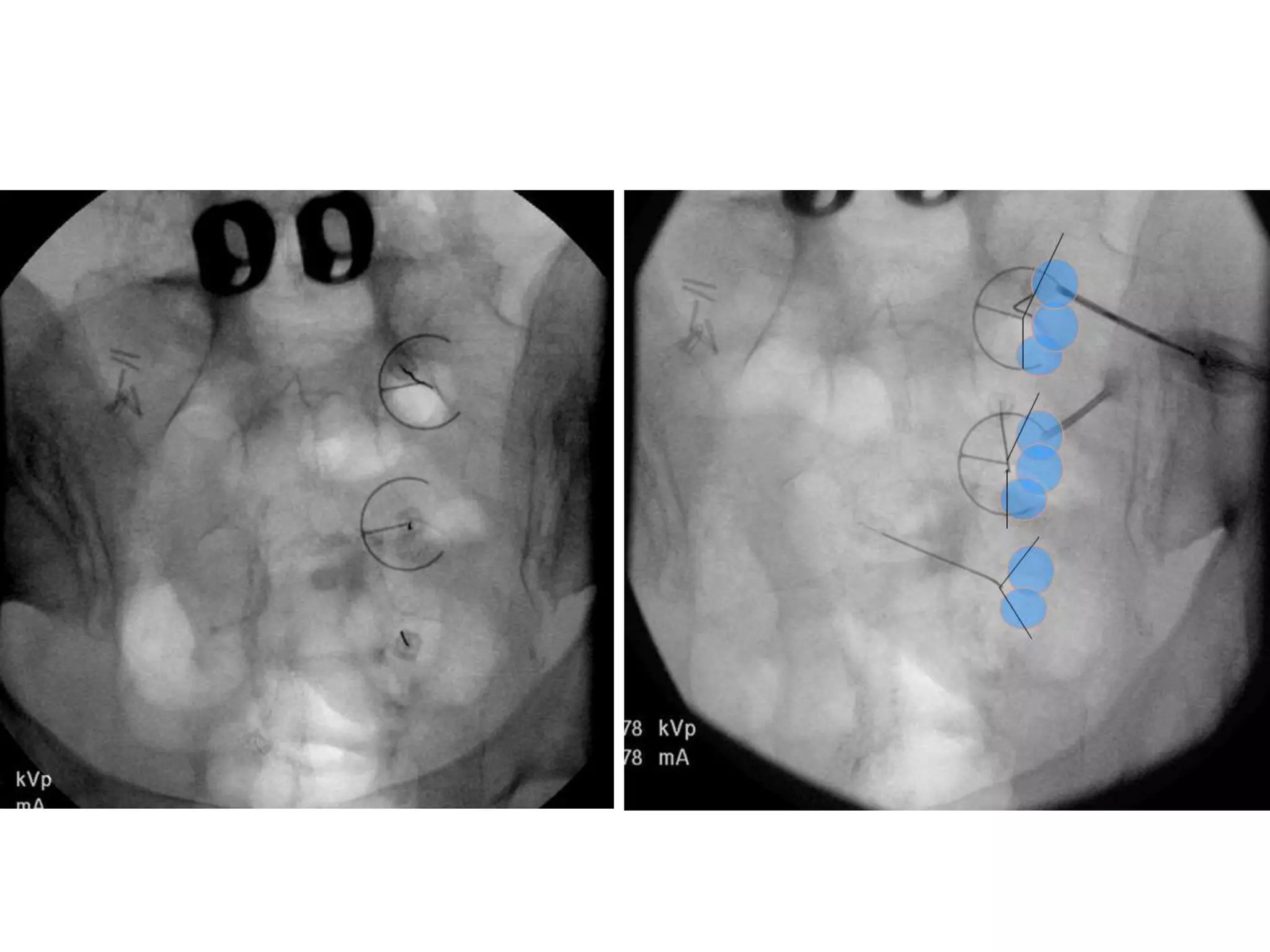
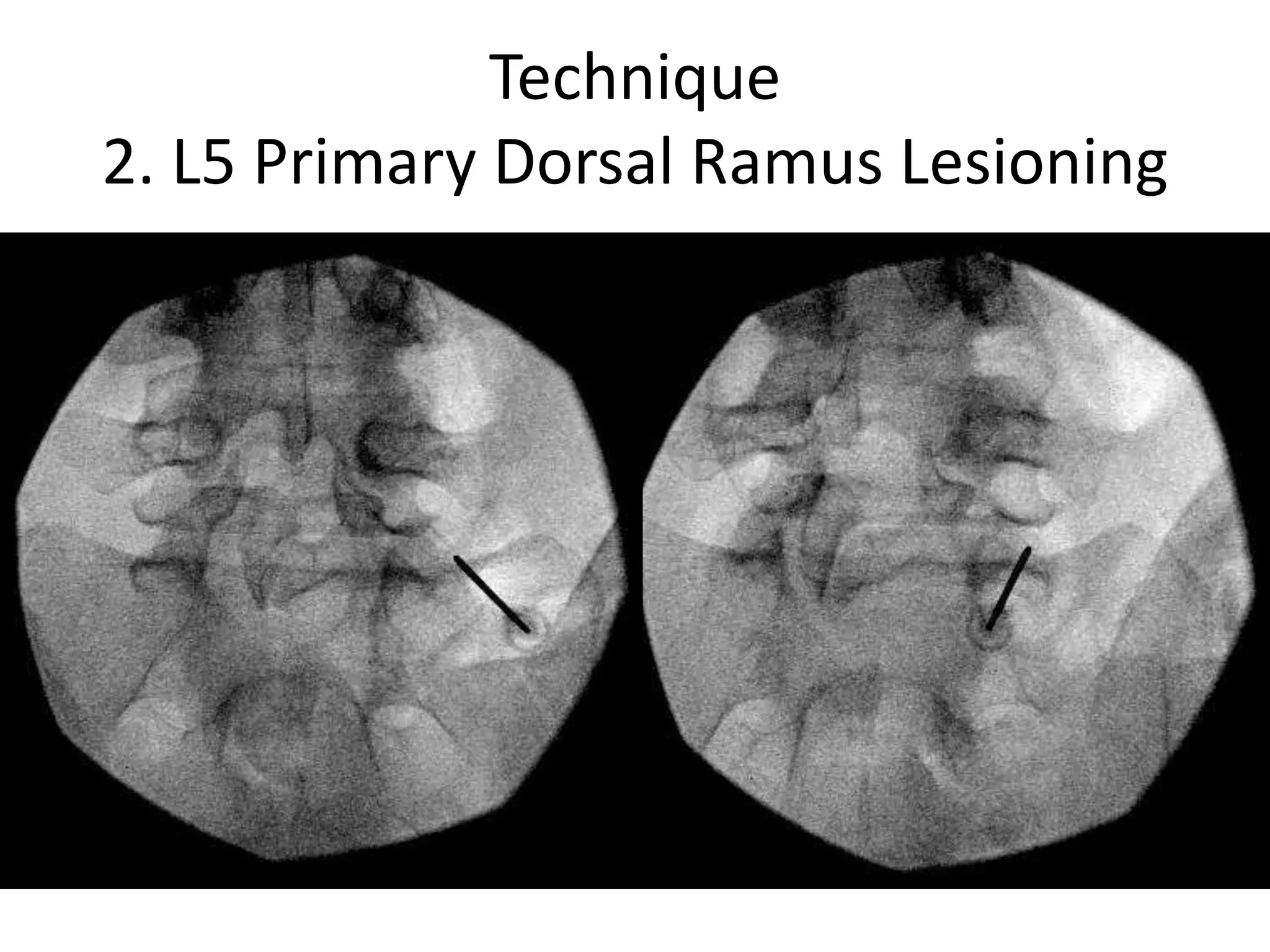
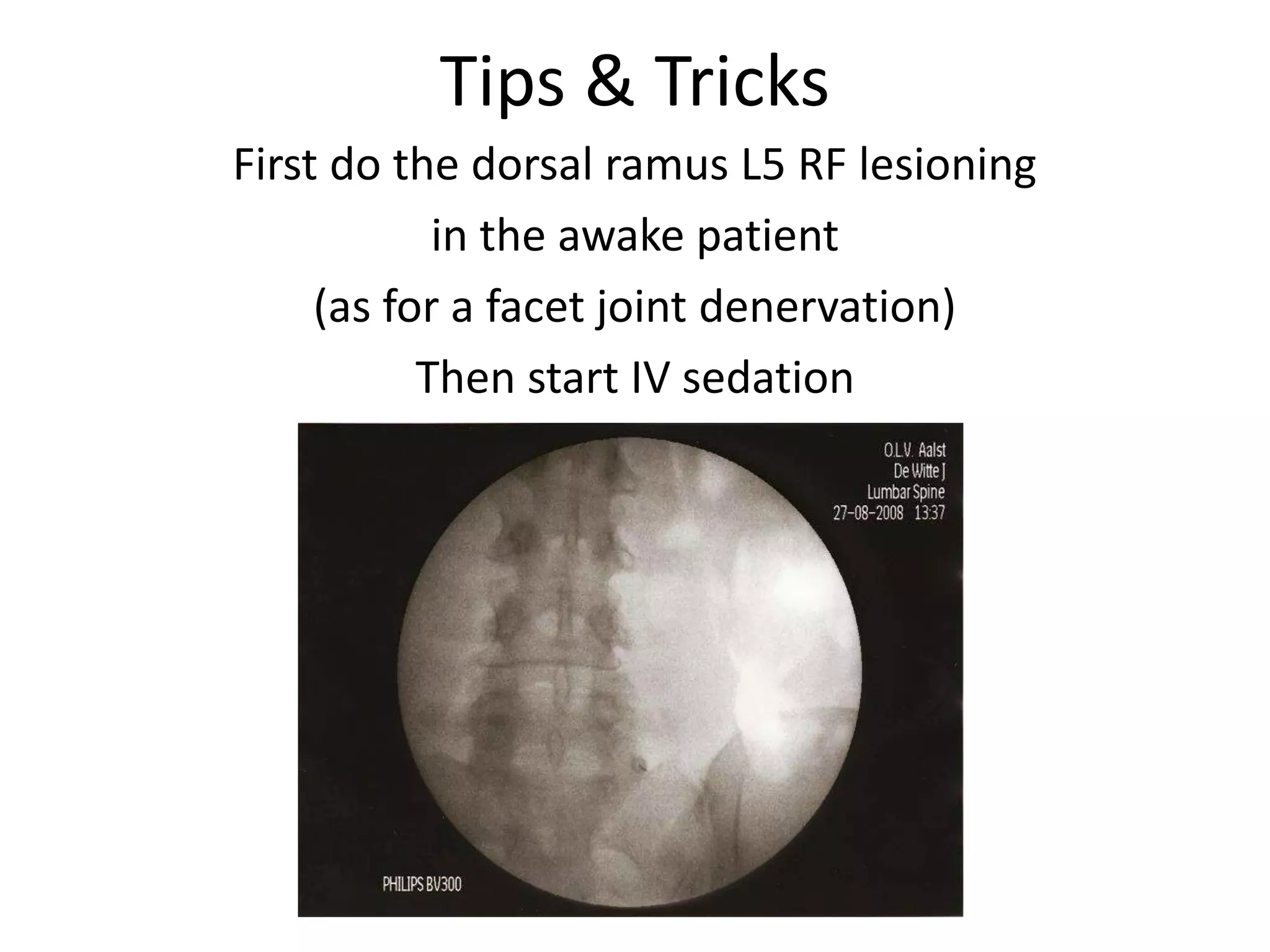
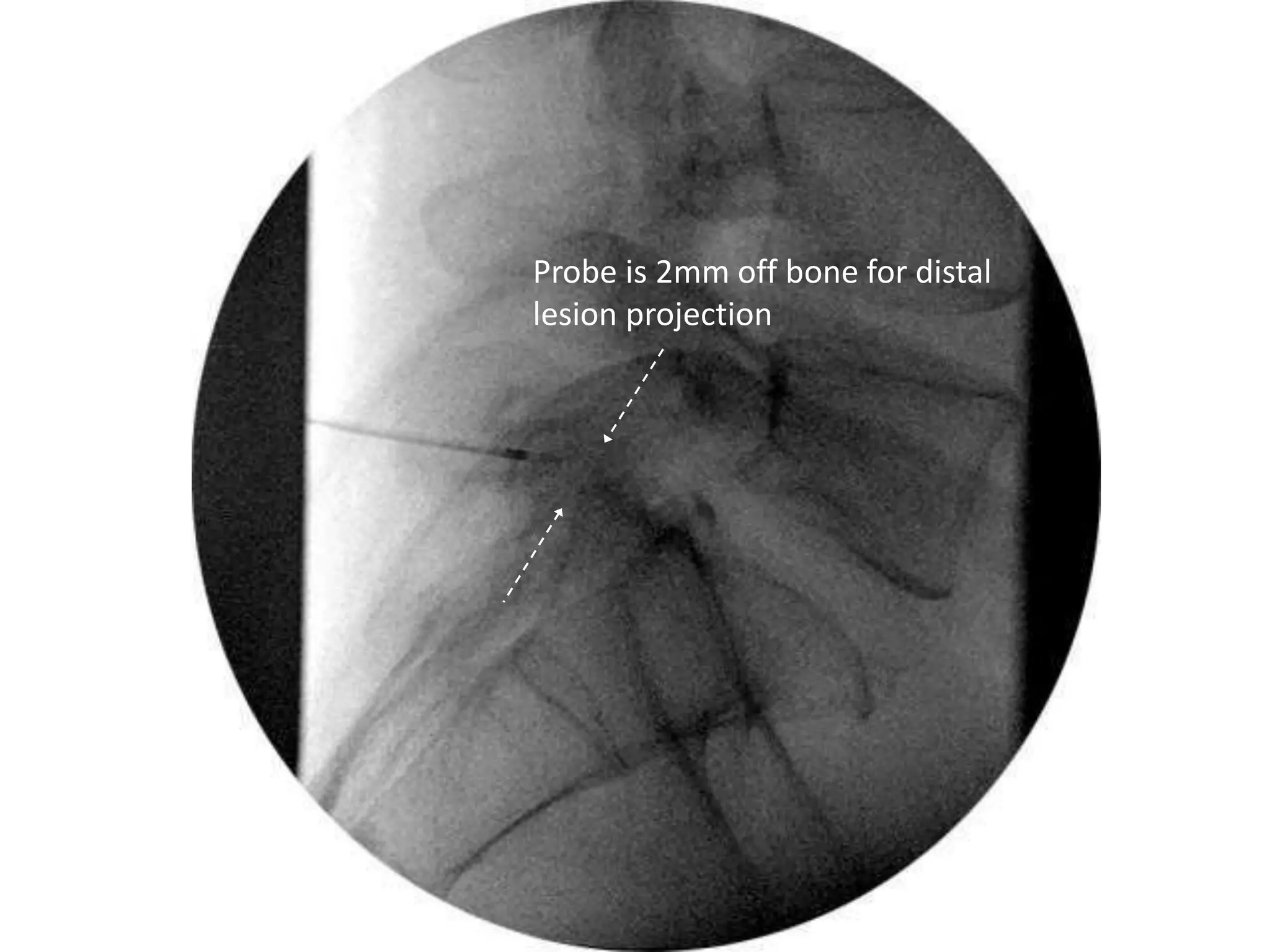
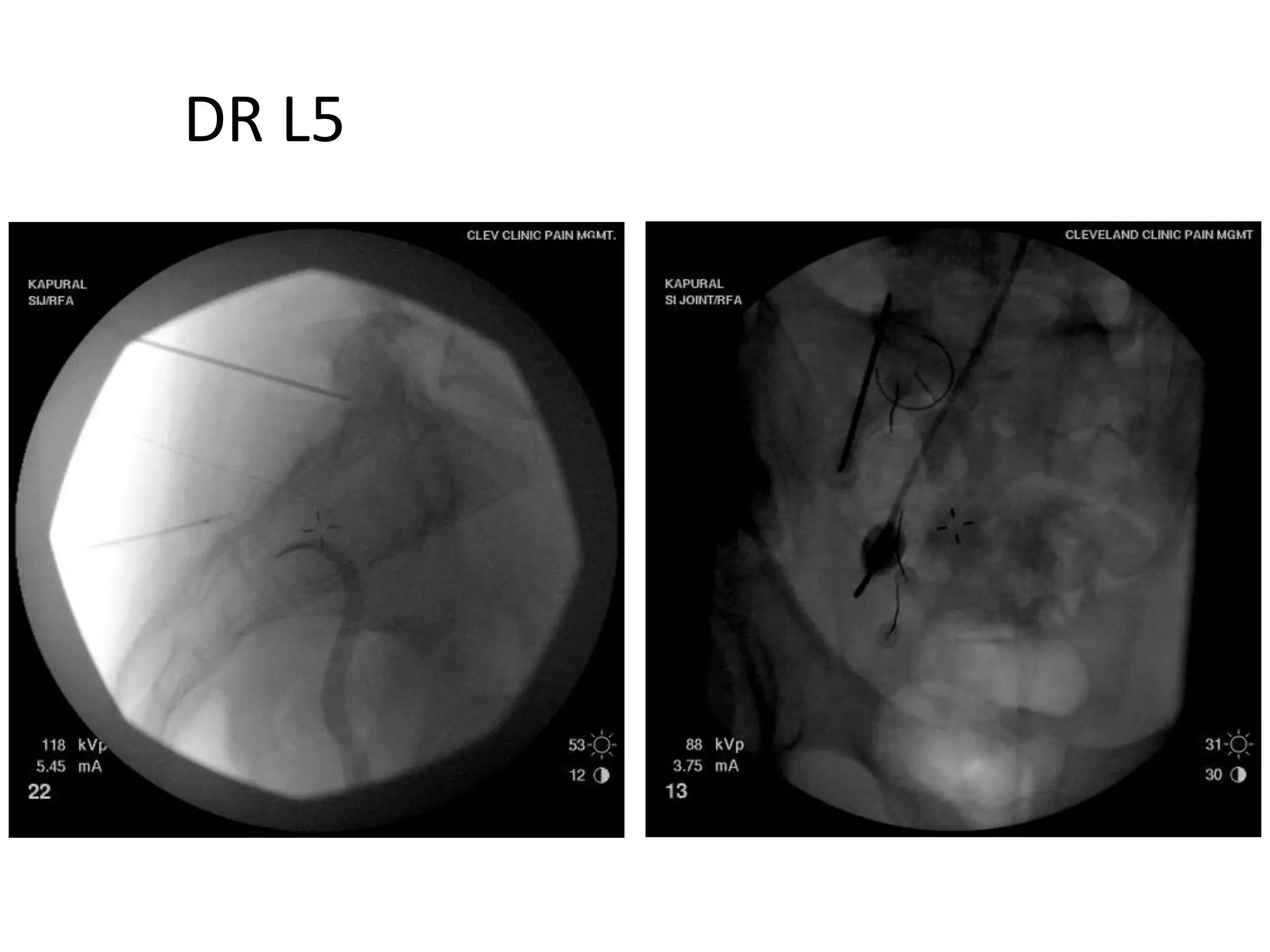
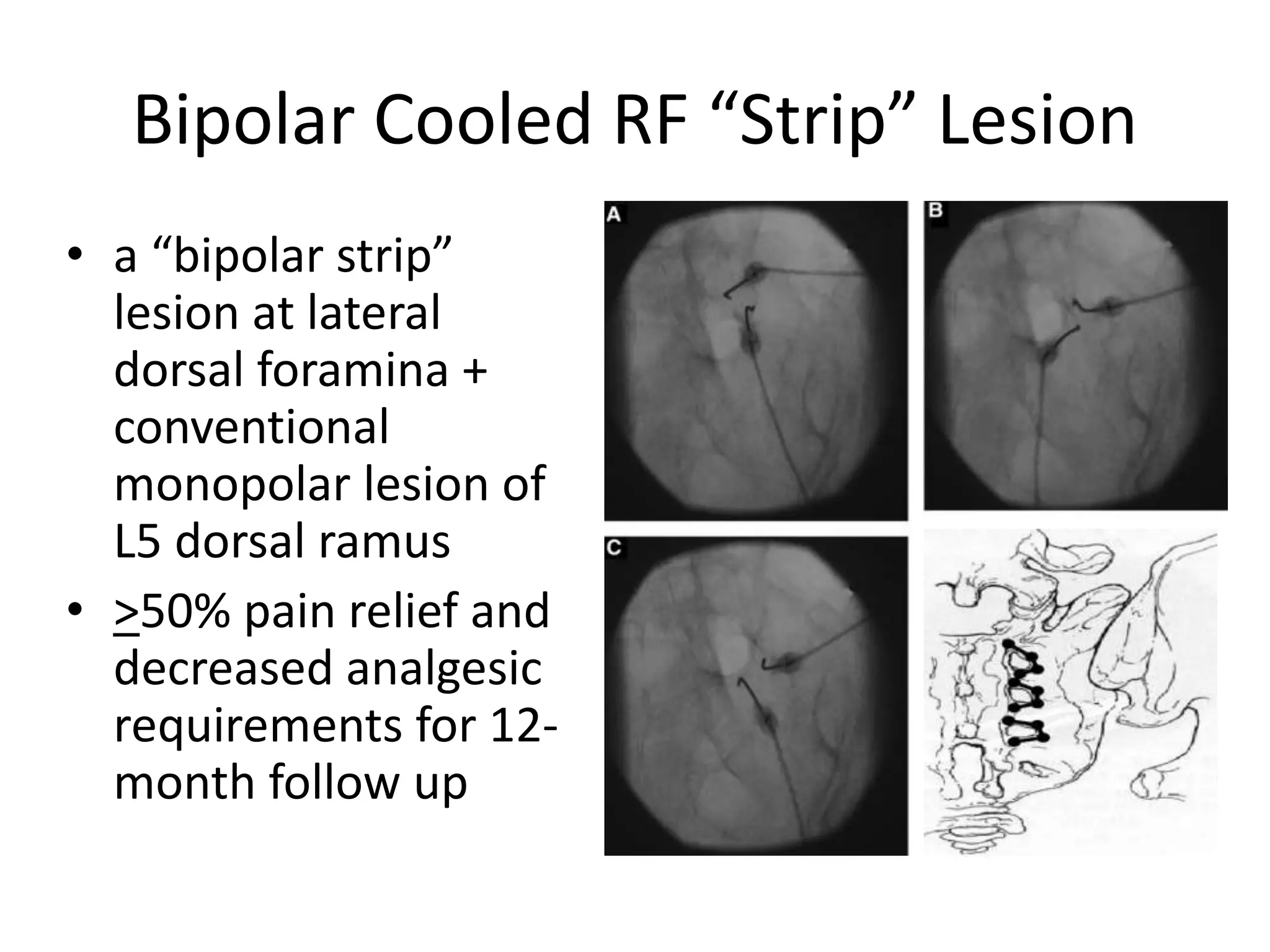
This document discusses radiofrequency denervation of the sacroiliac joint. It begins by describing the innervation of the SIJ, noting it is innervated by the posterior primary rami of S1 and S2 as well as occasional contributions from S3. It then discusses the diagnosis of SIJ pain, treatment options, and techniques for performing RFN of the SIJ including targeting the lateral branches of S1-S3 and the L5 dorsal ramus. Finally, it compares traditional RF and cooled RF techniques, noting cooled RF allows for large, controlled lesions and reduces risks compared to traditional RF.