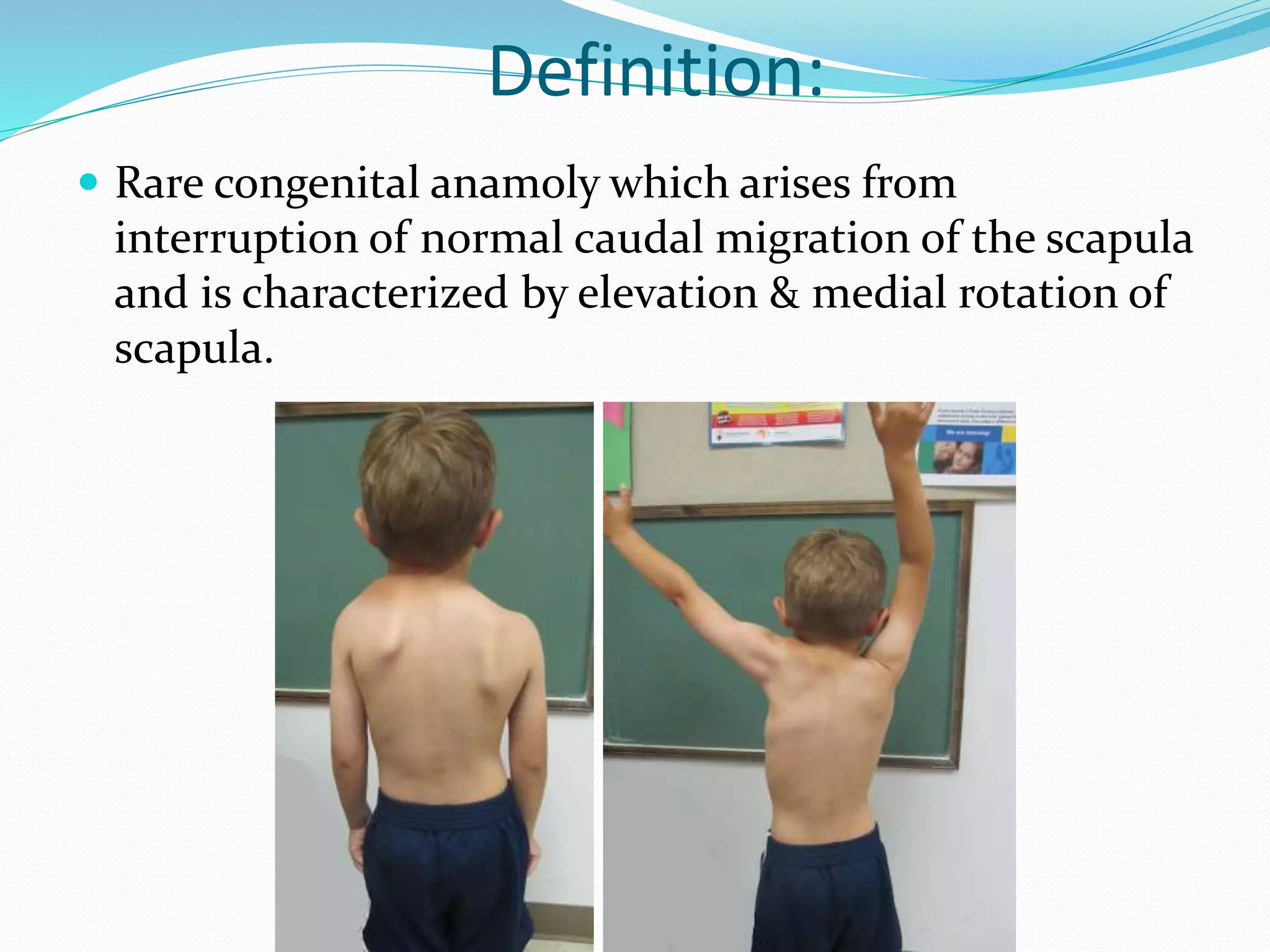
This document provides an overview of Sprengel's deformity, a rare congenital anomaly where the scapula is elevated and rotated medially. Key points:
- It results from interrupted migration of the scapula during embryonic development.
- Clinical features include an elevated shoulder, restricted shoulder movement, and sometimes scoliosis. Severity is graded based on elevation level.
- Diagnosis is made through x-rays showing elevated scapula position. CT scans can show associated bone anomalies.
- Surgical treatment aims to lower the scapula through muscle releases and reattachments, with the goal of improving function and asymmetry. Complications can include brachial plexus injury or sc