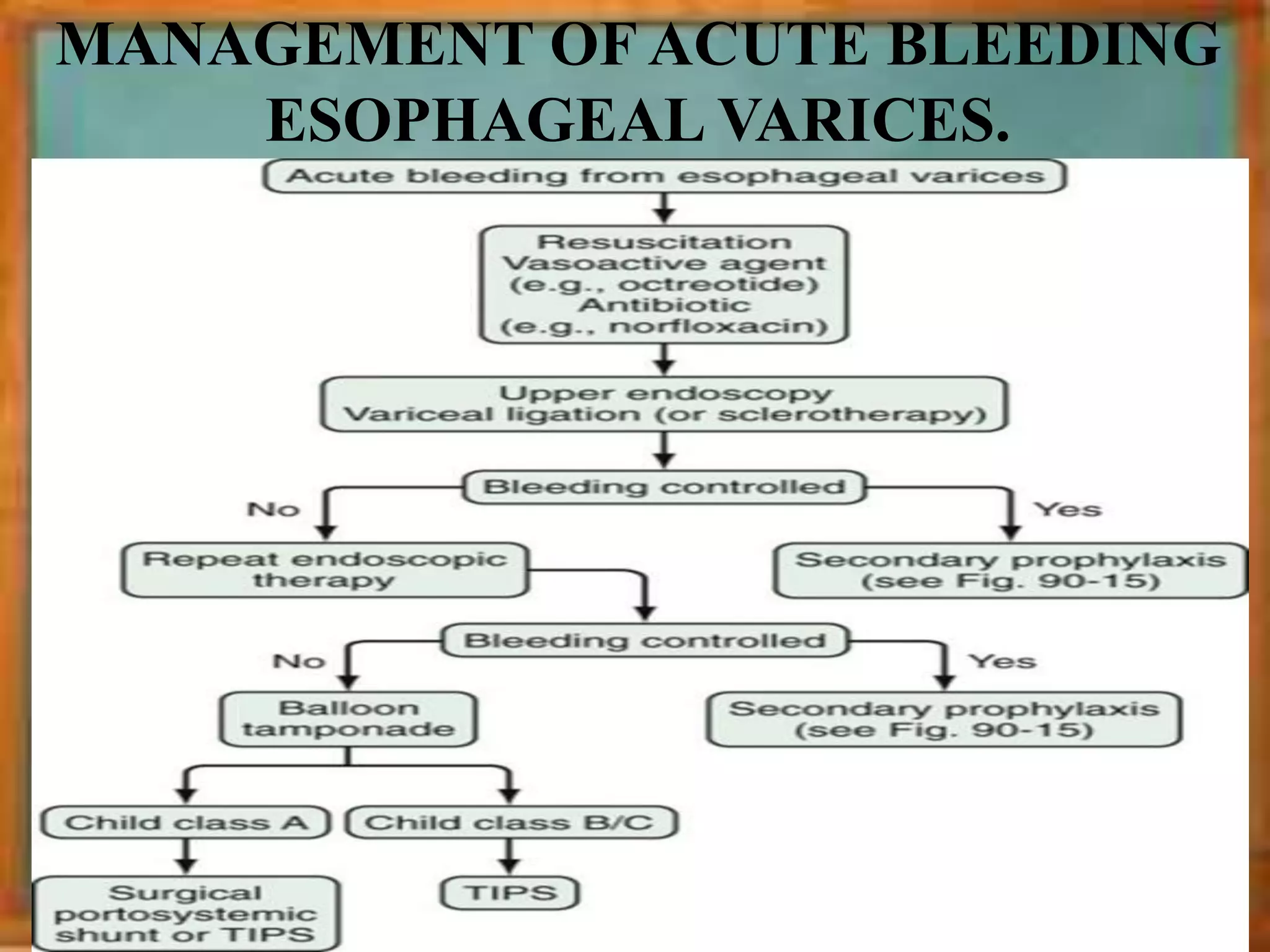
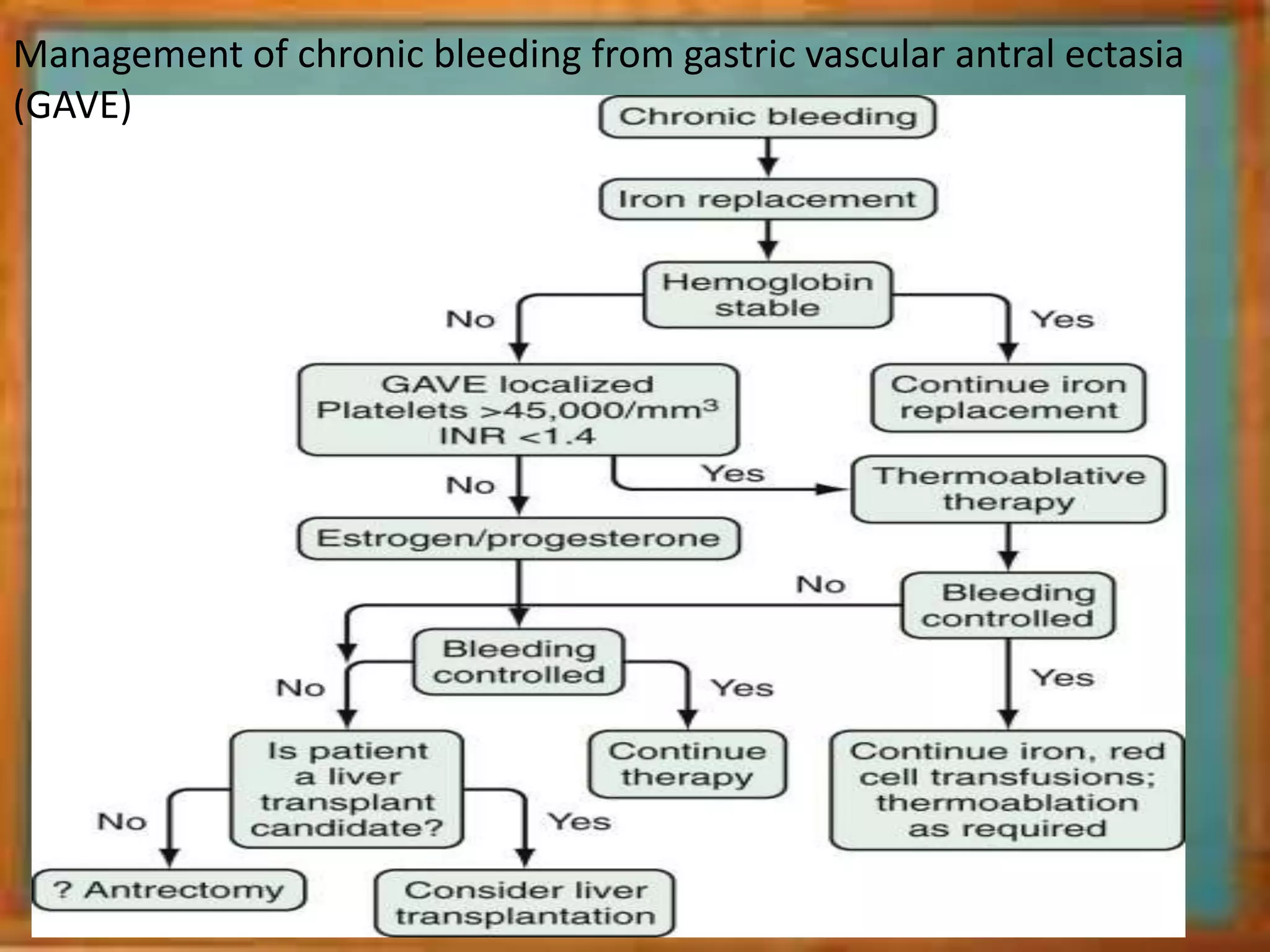
This document provides an overview of the approach to upper GI bleeding. It begins with definitions of terms like hematemesis, melena, and hematochezia. It then discusses the causes of upper GI bleeding, which can be variceal or non-variceal. For patients presenting with upper GI bleeding, the summary provides that history, physical exam, and investigations like endoscopy are important to determine the cause and guide management. Management may involve treating any active bleeding, administering PPIs for non-variceal causes, or using vasoactive agents, balloon tamponade, or endoscopic therapies for variceal bleeding.